Non-small cell lung cancer
Non-small cell lung cancer
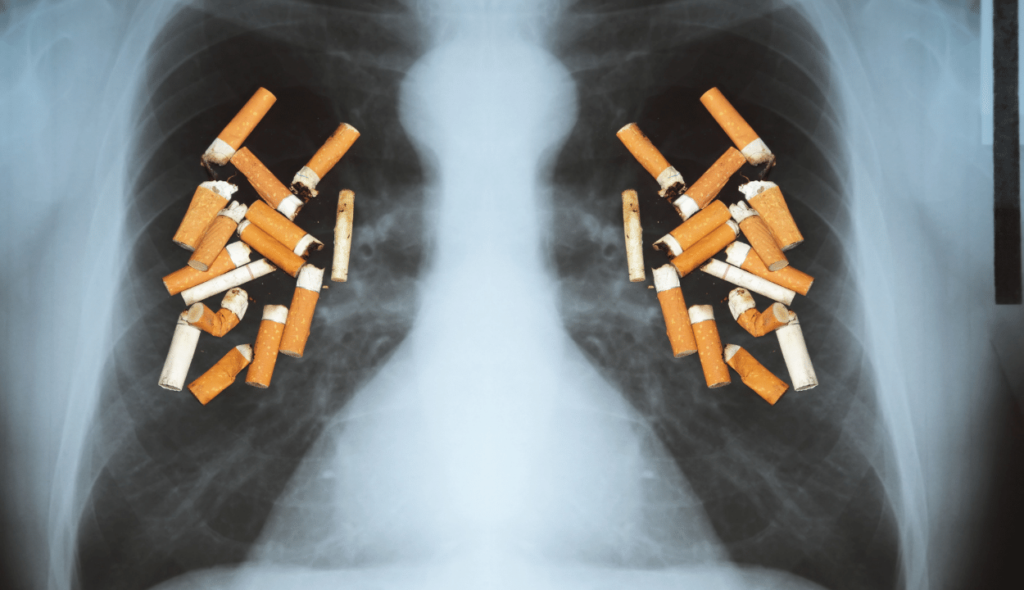
An estimated 2.3 million people worldwide are affected by lung cancer each year. Lung cancer can affect anyone, even though smoking cigarettes is the main cause. No matter the size, location, whether the cancer has spread, or how far it has spread, lung cancer is very treatable.
Because smoking has been linked to lung cancer, patients may worry that they won’t get any support or assistance because they assume that people would believe that their actions caused the sickness. The majority of smokers do not go on to acquire lung cancer, and not everyone who is diagnosed with the disease smoked cigarettes. Anyone can get the illness lung cancer. In actuality, the majority of persons who develop lung cancer today have never smoked or had quit smoking years ago.
Small cell lung cancer and non-small cell lung cancer are the two main subtypes of lung cancer (NSCLC). These two categories receive various treatments. This manual offers details on NSCLC. Visit a separate guide to learn more about small cell lung cancer. A detailed guide on lung neuroendocrine tumours is also available on this website.
NSCLC starts when normal lung cells transform and proliferate out of control to produce a mass known as a tumour, lesion, or nodule. This can start anywhere in the lung, and either a benign or malignant tumour may be present. A malignant lung tumour may expel cancer cells as it grows. These cells can travel through the blood or float in the lymph fluid that surrounds lung tissue. Lymph travels through lymphatic veins, which empty into lymph nodes, which serve as collection points.
The tiny, bean-shaped organs known as lymph nodes aid in the defence against infection. They can be found throughout the body, including in the lungs and the chest’s core. Lung cancer frequently spreads there first because of the natural direction of lymph flow out of the lungs, which is toward the centre of the chest. Metastasis is the term used to describe the spread of a cancer cell into a lymph node or through the bloodstream to another section of the body.
Types of NSCLC
There are different types of NSCLC. It is important to know the type of NSCLC because it can change treatment options. Doctors determine which type of NSCLC a person has based on the way the cancer looks under a microscope and the kind of cells the cancer starts in. The different types of NSCLC are:
Adenocarcinoma. This type of NSCLC begins in the epithelial cells that line the outside of the lungs. These cells make mucus. It is the most common type of lung cancer at about 40% of all NSCLC cases.
Squamous cell carcinoma. This type of cancer starts in the squamous cells, which are flat cells that line the inside of the lungs. About 30% of all NSCLC cases are squamous cell carcinoma.
Large cell carcinoma. The cells in large cell carcinoma do not look like adenocarcinoma or squamous cell carcinoma, instead they look like large cells. This is the least common type of NSCLC and as diagnostic tools get better, more large cell carcinomas are being classified as adenocarcinoma or squamous cell carcinoma.
Symptoms of NSCLC
The following signs or symptoms are possible in people with NSCLC. A symptom, such as exhaustion, nausea, or discomfort, is something that only the person experiencing it can recognise and explain. An indicator, such as a fever, rash, or increased pulse, is something that other people can spot and quantify. A medical issue can be described by its signs and symptoms taken together. Sometimes those who have NSCLC do not exhibit any of the symptoms listed below. Or, a medical disease other than cancer may be to blame for a symptom or sign’s occurrence.
Fatigue
Cough
Shortness of breath
Chest pain, if a tumor spreads to the lining of the lung or other parts of the body near the lungs
Loss of appetite
Coughing up phlegm or mucus
Coughing up blood
Unintentional weight loss
Hoarseness
Through a process known as metastasis, NSCLC can spread to any part of the body. The lymph nodes, more lung tissue, bones, brain, liver, and organs known as the adrenal glands located next to the kidneys are the places where it spreads most frequently. NSCLC metastatic disease may result in:
More breathing difficulties
Bone pain
Abdominal or back pain
Headache
Weakness
Seizures
Speech difficulties
Rarely, a lung tumor can release hormones that cause problems such as low blood sodium levels or high blood calcium levels
Metastases are not always to blame for symptoms like exhaustion, feeling lousy or ill, and appetite loss. A person may experience generalised illness if they have cancer anyplace in the body. Loss of appetite might result in muscle and weight loss. A person’s ability to breathe can become even worse from fatigue and weakness. Weakness and loss of motion are also caused by muscle loss.
In the event that cancer is discovered, managing symptoms is still a crucial component of care and treatment. Palliative care or supportive care are two names for this. It frequently begins as soon as a diagnosis is made and continues during therapy. Make sure to discuss all of your symptoms, especially any new ones or ones that have changed, with your medical staff.
Diagnosis of NSCLC
There are many tests used for diagnosing NSCLC. Not all tests described here will be used for every person. Your doctor may consider these factors when choosing a diagnostic test:
The type of cancer suspected
Your signs and symptoms
Your age and general health
The results of earlier medical tests
Imaging tests
In the treatment of those with NSCLC, imaging tests are crucial. But no test is 100% accurate, and no scan can identify NSCLC. Only a biopsy can achieve that (see below). For a complete picture of where the cancer started and whether or not it has spread, chest x-ray and scan results must be paired with a person’s medical history, a physical examination, blood tests, and information from the biopsy.
Computed tomography (CT or CAT) scan:
The size and location of a lung tumour and/or lung cancer metastases can be seen by doctors thanks to the pictures produced by a CT scan. Using x-rays acquired from various angles, a CT scan creates images of the interior of the body. These images are combined by a computer to create a detailed, three-dimensional image that reveals any anomalies or malignancies. The tumor’s size can be determined via a CT scan. To offer more detail on the image, a contrast medium, a specific dye, is occasionally administered prior to the scan. This dye can be administered intravenously or as a tablet or liquid for ingestion.
Positron emission tomography (PET) scan:
A PET-CT scan, which combines a PET scan with a CT scan (see above), is the norm. Your doctor might, however, simply call this treatment a PET scan. Making images of the organs and tissues inside the body is possible with a PET scan. The patient receives a little injection of a radioactive sugar compound. The cells that consume the most energy absorb this sugar molecule. Cancer absorbs more of the radioactive substance since it tends to use energy actively. The material is then detected by a scanner, which creates images of the interior of the body.
Magnetic resonance imaging (MRI) scan:
Additionally, an MRI generates images that let medical professionals determine the size and location of lung tumours and/or lung cancer metastases. Instead than using x-rays, an MRI creates precise images of the body using magnetic fields. Before the scan, a specific dye called a contrast medium is administered to produce a crisper image. This dye can be administered intravenously or as a tablet or liquid for ingestion. To capture images of moving body parts, such as your lungs, which move with each breath you take, MRI scanning does not perform well. Because of this, MRI is rarely utilised to examine the lungs. Finding lung cancer that has spread to the brain or bones could be useful.
Bone scan:
During a bone scan, a radioactive tracer is used to examine the interior of the bones. The tracer contains too little radiation to be dangerous. A patient receives the tracer by injection into a vein. A specialised camera finds it where it accumulates on the bone. Areas of injury, such as those brought on by cancer, show out on the image and healthy bone appears lighter to the camera. To detect NSCLC that has progressed to the bones, PET scans (see above) have taken the place of bone scans.
Biopsy:
A biopsy is the removal of a tiny sample of tissue for microscopic analysis. To identify the NSCLC subtype and perform additional molecular testing, a bigger tumour sample is beneficial (see below). Another biopsy might be required if not enough of the tumour was removed to perform these tests. A pathologist examines the sample following the biopsy (s). A pathologist is a medical professional who focuses on analysing lab results and assessing cells, tissues, and organs to identify diseases.
Bronchoscopy:
A small, flexible tube with a light on the end is inserted via the mouth or nose, down the major windpipe, and into the breathing passages of the lungs during a bronchoscopy. This treatment may be carried out by a surgeon or a pulmonologist. A physician who focuses on the identification and management of lung conditions is known as a pulmonologist. The doctor can see within the lungs thanks to the tube. Small tools inside the tube might collect fluid or tissue samples for the pathologist to evaluate. Using an ultrasound to direct the bronchoscopy, lymph nodes are frequently inspected, and samples are frequently taken. An endobronchial ultrasonography is what this is (EBUS). During a bronchoscopy, patients get a minimal amount of anaesthetic. Medication called anaesthesia is used to numb pain perception.
Needle aspiration/core biopsy:
A particular kind of radiologist known as an interventional radiologist numbs the skin before removing a lung tumour sample for analysis. Depending on how large of a sample is required, either a smaller or larger needle might be used. The medical professional uses the needle to take a sample of tissue for analysis. The radiologist frequently utilises a fluoroscope, a specialised x-ray device, or a chest CT scan to guide the needle. Generally speaking, a core biopsy yields more tissue than a needle aspiration. As previously said, medical professionals now know that additional tissue is required for molecular testing and diagnosis of NSCLC.
Thoracentesis:
After numbing the skin on the chest, a needle is inserted through the chest wall and into the space between the lung and the wall of the chest where fluid can collect. The fluid is removed and checked for cancer cells by the pathologist.
Thoracoscopy:
The patient is given general anaesthesia before this surgery is carried out in the operating room. A surgeon can introduce a special tool and a tiny video camera through a small cut in the skin of the chest wall to help with the inspection of the inside of the chest. Patients must undergo general anaesthesia for this operation, however due to the smaller incisions required during a thoracoscopy, recovery time may be shortened. Video-assisted thoracoscopic surgery, or VATS, is another name for this treatment. Robotic-assisted surgery is a different form of minimally invasive procedure that could be used in place of a thoracoscopy.
Mediastinoscopy:
The patient is given general anaesthesia for this operation, which is done in the operating room. A small incision is made at the top of the breastbone to allow the surgeon access to the lymph nodes underneath the breastbone for examination and sample collection. The operating room is used for this surgery, which also calls for general anaesthesia.
Thoracotomy:
The patient is given general anaesthesia, and the procedure is carried out in an operating room. Next, a surgeon makes a chest incision to view the lung up close and collect tissue samples for analysis. A thoracotomy may be required to entirely remove a lung tumour even though it is rarely used to identify lung cancer.
Stages of NSCLC
Stage 0 (zero) and stages I through IV make up the NSCLC’s five stages (1 through 4). Finding out if the cancer can be surgically totally removed is one technique to evaluate the NSCLC stage. The surgeon must remove the cancer, the healthy lung tissue surrounding it, and frequently any neighboring lymph nodes in order to entirely eradicate the lung cancer.
Stage 0
This is called in situ disease, meaning the cancer is “in place” and has not grown into nearby normal lung tissues or spread outside the lung.
Stage I
A stage I lung cancer is a small tumor that has not spread to any lymph nodes. Stage I is divided into 2 substages based on the size of the tumor:
Stage IA tumors are 3 centimeters (cm) or less in size. Stage IA tumors may be further divided into IA1, IA2, or IA3 based on the size of the tumor.
Stage IB tumors are more than 3 cm but 4 cm or less in size.
Stage II
Stage II lung cancer is divided into 2 substages:
A stage IIA cancer describes a tumor larger than 4 cm but 5 cm or less in size that has not spread to the nearby lymph nodes.
Stage IIB lung cancer describes a tumor that is 5 cm or less in size that has spread to the lymph nodes within the lung, called the N1 lymph nodes. A stage IIB cancer can also be a tumor more than 5 cm wide that has not spread to the lymph nodes.
Usually, stage II tumors can be removed with surgery, but often additional treatments are recommended.
Stage III
Lung tumours in stage III might be stage IIIA, stage IIIB, or stage IIIC. The size of the tumour and the lymph nodes to which the malignancy has progressed determine the stage. Cancers in stage III have not spread to other far-off areas of the body.
The doctor will check to see whether the cancer has not spread to other body parts if stage III NSCLC is detected. A physical examination, evaluation of the patient’s medical history, a CT scan of the chest and upper abdomen, a PET-CT scan, and an MRI of the brain are all advised by ASCO for this evaluation (see Diagnosis). For some individuals, endoscopy or surgery may be required to check the lymph nodes for malignancy. According on the stage, other characteristics, and any additional medical conditions the patient may have, a team of cancer care specialists usually collaborates to determine the best course of action.
It may be challenging or perhaps impossible to entirely remove the tumour with surgery alone for many stage IIIA and stage IIIB malignancies. In general, stage IIIC tumours cannot be removed surgically and may require treatment with a chemotherapy and radiation regimen followed by immunotherapy. For instance, the lymph nodes inside the chest, outside the lung, may have been affected by the lung cancer. Or the lung’s adjacent structures may have been affected by the tumor’s growth. It is less probable that the surgeon will be able to totally remove the cancer in either scenario. Systemic therapy and radiation therapy are frequently effective treatments for stage III tumours that cannot be treated surgically.
Stage IV
Stage IV lung cancer denotes the spread of the disease to many sites in the other lung, the fluid around the lung or the heart, or distant sections of the body through the bloodstream. Cancer can spread to any part of the body once it enters the bloodstream. NSCLC is more likely to extend to the liver, adrenal glands, bones, and brain nevertheless. There are two substages of stage IV NSCLC:
Cancer at stage IVA has spread to one place outside of the chest or within the chest.
Stage IVB has expanded to more than one location in one organ, or to more than one organ, outside of the chest.
For the majority of stage IIIB, IIIC, or IV lung tumours, surgery is typically not an option. When lung cancer has reached key chest structures or the lymph nodes above the collarbone, removal can be challenging. The primary breathing tubes that lead to the lungs, the heart, and massive blood veins are a few examples. In these cases, the doctor will carefully assess if surgery is an option or whether to suggest alternative therapies. If the tumour cannot be entirely eliminated, surgery is typically not advised. However, surgery and/or radiation therapy may be recommended to treat the remaining cancerous areas in some stage IV lung cancer patients who respond well to treatment.
Treatment of NSCLC
In the context of cancer care, many medical specialties frequently collaborate to develop a patient’s comprehensive treatment plan, which incorporates a variety of therapies. A interdisciplinary team is what this is. A wide range of other medical specialists, including physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counsellors, nutritionists, and others, are part of cancer care teams.
There are 5 main ways to treat NSCLC:
Surgery
Chemotherapy
Immunotherapy
Following a summary of the typical treatment plans by stage, the typical forms of treatments utilised for NSCLC are presented. Treatment for symptoms and side effects is a crucial component of your care strategy for cancer.
The type and stage of the cancer, potential side effects, the patient’s preferences, and general health are just a few of the variables that can affect the recommended course of treatment. Spend some time researching all of your therapy options, and make sure to clarify anything that is unclear. Discuss with your doctor the intended outcomes of each course of treatment as well as what to anticipate during it. “Shared decision-making” refers to these types of discussions. When you and your doctors collaborate to select therapies that meet the objectives of your care, this is known as shared decision-making. Given the variety of available treatments for NSCLC, shared decision-making is especially crucial.
Surgery in NSCLC
The entire lung tumour as well as any adjacent lymph nodes in the chest are to be removed during surgery. A margin or border of healthy lung tissue must be present around the tumour when it is removed. A “negative margin” means that no cancer was discovered in the healthy tissue surrounding the tumour when the pathologist examined the lung or a portion of the lung that was surgically removed. An expert in utilising surgery to treat cancer is known as a surgical oncologist. To operate on lung cancer, a thoracic surgeon has received specialised training.
The following types of surgery may be used for NSCLC:
Lobectomy. The lungs have 5 lobes, 3 in the right lung and 2 in the left lung. A lobectomy is the removal of an entire lobe of the lung. It is currently thought to be the most effective type of surgery, even when the lung tumor is very small. Clinical trials are underway to study if less extensive surgeries have similar outcomes for tumors that are less than or equal to 2 centimeters.
A wedge resection. If the surgeon cannot remove an entire lobe of the lung, the surgeon can remove the tumor, surrounded by a margin of healthy lung.
Segmentectomy. This is another way to remove the cancer when an entire lobe of the lung cannot be removed. In a segmentectomy, the surgeon removes the portion of the lung where the cancer developed. Typically, more lung tissue and lymph nodes are removed during a segmentectomy compared to a wedge resection.
Pneumonectomy. If the tumor is close to the center of the chest, the surgeon may have to remove the entire lung. A pneumonectomy has more risks than a lobectomy and your doctor will need to consider the health of your heart and lungs before performing this surgery.
Radiation therapy
High energy x-rays or other particles are used in radiation therapy to kill cancer cells. You will visit a radiation oncologist if you require radiation therapy. A physician who specialises in administering radiation treatment to treat cancer is known as a radiation oncologist. External-beam radiation therapy, or radiation delivered from a machine outside the body, is the most used form of radiation therapy. A radiation therapy regimen, often known as a schedule, typically has a predetermined number of sessions spread out over a predetermined amount of time. This can last anywhere from a few days to several weeks.
Radiation therapy, like surgery, cannot be used to treat cancer that has spread widely. Only the cancer cells that are directly in the radiation beam’s path are killed by radiation therapy. The healthy cells that are in its path are likewise harmed. Large parts of the body cannot be treated because of this. Stereotactic body radiation therapy (SBRT) or intensity-modulated radiation therapy (IMRT) may occasionally be employed. In order to reduce the risk of injuring healthy body components, these radiation therapy techniques use CT scans or PET scans to precisely plan where to direct the radiation beam. When surgery is not an option, it may be utilised for tiny tumours and early-stage disease, albeit it is not a choice for all individuals.
Stereotactic radiation therapy may be used as an alternative to surgery for some patients with Stage I NSCLC or those who are unable to undergo surgery.
Chemotherapy
Chemotherapy is the use of medications to kill cancer cells, typically by preventing the growth, division, and production of new cancer cells. For those with lung cancer in any stage, it has been demonstrated to prolong and improve quality of life.
A chemotherapy regimen, often known as a schedule, typically entails a defined number of cycles administered over a predetermined amount of time. Which medications are suggested for chemotherapy depends on the type of lung cancer you have, such as adenocarcinoma or squamous cell carcinoma.
Two, three, or one drug may be used alone or in combination with other medications to treat lung cancer. Several popular medicines include:
Carboplatin (available as a generic drug)
Cisplatin (available as a generic drug)
Docetaxel (Taxotere)
Etoposide (available as a generic drug)
Gemcitabine (Gemzar)
Nab-paclitaxel (Abraxane)
Paclitaxel (Taxol)
Pemetrexed (Alimta)
Vinorelbine (Navelbine)
Targeted therapy
A treatment known as targeted therapy specifically targets the cancer’s unique genes, proteins, or tissue environment that promotes the growth and survival of the disease. This form of therapy prevents the development and spread of cancer cells while minimising harm to healthy cells.
The targets of every tumour vary. Your doctor may order tests to determine the genes, proteins, and other components of the tumour in order to choose the best course of treatment. In the cancer cells of some lung tumours, aberrant proteins are present in extremely high concentrations. When possible, this enables doctors to provide each patient with the most beneficial care. Additionally, new medicines that target particular molecular targets are being discovered through research studies.
Due to the pace of scientific discovery, tailored therapy for NSCLC is changing quickly. Clinical trials are currently looking at new targeted medicines. Discuss any further choices you may have with your doctor.
NSCLC targeted therapy includes:
Due to the pace of scientific discovery, tailored therapy for NSCLC is changing quickly. Clinical trials are currently looking at new targeted medicines. Discuss any further choices you may have with your doctor.
NSCLC targeted therapy includes:
Epidermal growth factor receptor (EGFR) inhibitors. About 10%-15% of all lung cancers are EGFR-positive. Researchers have found that drugs that block EGFR may be effective for stopping or slowing the growth of lung cancer when the cancer cells have EGFR mutations. The following EGFR inhibitors are approved by the FDA:
Afatinib (Gilotrif)
Dacomitinib (Vizimpro)
Entrectinib (Rozlytrek)
Erlotinib (Tarceva)
Gefitinib (Iressa)
Osimertinib (Tagrisso)
Drugs targeting the EGFR exon 20 insertion. Some people have a specific change to the EGFR gene in the exon 20. This is called an EGFR exon 20 insertion. The following drugs have been approved to target EGFR exon 20 insertion:
Amivantamab (Rybrevant)
Mobocertinib (Exkivity)
Anaplastic lymphoma kinase (ALK) inhibitors. ALK is a protein that is a part of the cell growth process. When present, this helps cancer cells grow. ALK inhibitors help stop this process. Changes in the ALK gene are found in about 4% of people with NSCLC. The following drugs are currently available to target this genetic change:
Alectinib (Alecensa)
Brigatinib (Alunbrig)
Ceritinib (Zykadia)
Crizotinib (Xalkori)
Lorlatinib (Lorbrena)
Drugs targeting ROS1 fusion. Rare changes to the ROS1 gene called ROS1 fusion or ROS1 rearrangement can cause problems with cell growth and cell differentiation. Cell differentiation is the process by cells use to change from one type of cell into another. ROS1 fusion is found in 1% to 2% of people with lung cancer. Drugs targeting changes to the ROS1 gene include:
Ceritinib (Zykadia)
Crizotinib (Xalkori)
Entrectinib (Rozlytrek)
Drugs targeting KRAS G12C mutations. The KRAS G12C is one of the most common genetic mutations found in people with NSCLC. About 20 to 25% of people with lung cancer have a KRAS mutation. One drug is approved to target KRAS G12C mutations:
Sotorasib (Lumakras)
Drugs targeting NTRK fusion. This type of genetic change is found in a range of cancers and causes cancer cell growth. It is rare in lung cancer (less than 1%). One drug is approved to target NTRK fusion:
Larotrectinib (Vitrakvi)
Drugs targeting BRAF V600E mutations. The BRAF gene makes a protein that is involved in cell growth and can cause cancer cells to grow and spread. BRAF mutations have been found in 4% of NSCLC cases. BRAF V600E mutations can be targeted with a combination of the following drugs:
Dabrafenib (Tafinlar)
Trametinib (Mekinist)
Drugs targeting MET exon 14 skipping. MET exon 14 skipping is a genetic mutation found in over 3% of NSCLC cases. Drugs approved to treat MET exon 14 skipping include:
Capmatinib (Tabrecta)
Tepotinib (Tepmetko)
Drugs targeting RET fusion. Up to 2% of all NSCLC cases are RET fusion positive. Drugs approved to target RET fusion positive NSCLC include:
Pralsetinib (Gavreto)
Selpercatinib (Retevmo)
Anti-angiogenesis therapy. Anti-angiogenesis therapy stops angiogenesis, which is the process of making new blood vessels. Because a tumor needs the nutrients delivered by blood vessels to grow and spread, the goal of anti-angiogenesis therapies is to “starve” the tumor. The following anti-angiogenic drugs may be options for lung cancer:
Bevacizumab (Avastin, Mvasi), in combination with chemotherapy and atezolizumab (Tecentriq), an immunotherapy drug (see below)
Ramucirumab (Cyramza), in combination with the chemotherapy drug docetaxel
Side effects of targeted therapy depend on the drug(s) you’ve been prescribed. They are different from side effects commonly caused by chemotherapy and they can be serious. For example, targeted therapy can cause skin, hair, nail, or eye problems. Talk with your doctor about possible side effects for a specific medication and how they can be managed.
Immunotherapy
Immunotherapy, also called biologic therapy, is designed to boost the body’s natural defenses to fight the cancer. It uses materials made either by the body or in a laboratory to improve, target, or restore immune system function.
People who receive treatment using immunotherapy for NSCLC may receive only one drug, a combination of immunotherapy drugs, or it may be combined with chemotherapy. When advanced NSCLC cannot be treated with a targeted therapy (see above), immunotherapy or immunotherapy plus chemotherapy is often the preferred initial treatment.
There are different ways immunotherapy can use the body’s immune system to treat cancer.
Drugs that block the PD-1 pathway. The PD-1 pathway may be very important in the immune system’s ability to control cancer growth. Blocking this pathway with PD-1 and PD-L1 antibodies has stopped or slowed the growth of NSCLC for some patients. The following immunotherapy drugs block this pathway and are approved to treat NSCLC:
Atezolizumab (Tecentriq)
Durvalumab (Imfinzi)
Cemiplimab-rwlc (Libtayo)
Nivolumab (Opdivo)
Pembrolizumab (Keytruda)
Drugs that block the CTLA-4 pathway. Another immune pathway that may be targeted is the CTLA-4 pathway. The FDA has approved one drug that blocks this pathway to treat NSCLC:
- Ipilimumab (Yervoy)
Ipilimumab is given in combination with nivolumab, which blocks the PD-1 pathway. This combination can also be used with chemotherapy.
Different types of immunotherapy can cause different side effects but, in general, severe side effects are less common than with chemotherapy. Immune-related side effects are possible with immunotherapy and include skin reactions, flu-like symptoms, diarrhea, shortness of breath from lung inflammation, and weight changes. The risk of immune-related side effects is higher if a PD-1/PD-L1 inhibitor is combined with a CTLA-4 inhibitor. Talk with your doctor about possible side effects for the immunotherapy recommended for you.
Take second opinion on NSCLC treatment
- Comments Closed
- June 26th, 2022



Latest Posts
- LungVax: Lung cancer vaccine
- Successful CRISPR Gene Therapies in Practice: Case Studies
- Gamma Delta (γδ) T cells as a potential treatment for glioblastoma
- World-first lung cancer vaccine trials started in seven countries
- Lazertinib with amivantamab-vmjw is approved by the USFDA for non-small lung cancer
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (58)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (790)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (104)
- Cervical cancer (41)
- Chemotherapy (37)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (20)
- Endometrial cancer (10)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (2)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (48)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (45)
- Liver cancer (94)
- Lung cancer (69)
- Lymphoma (46)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (23)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (12)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (8)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (747)
- Treatment in China (647)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview