Hairy cell leukemia
Hairy cell leukemia
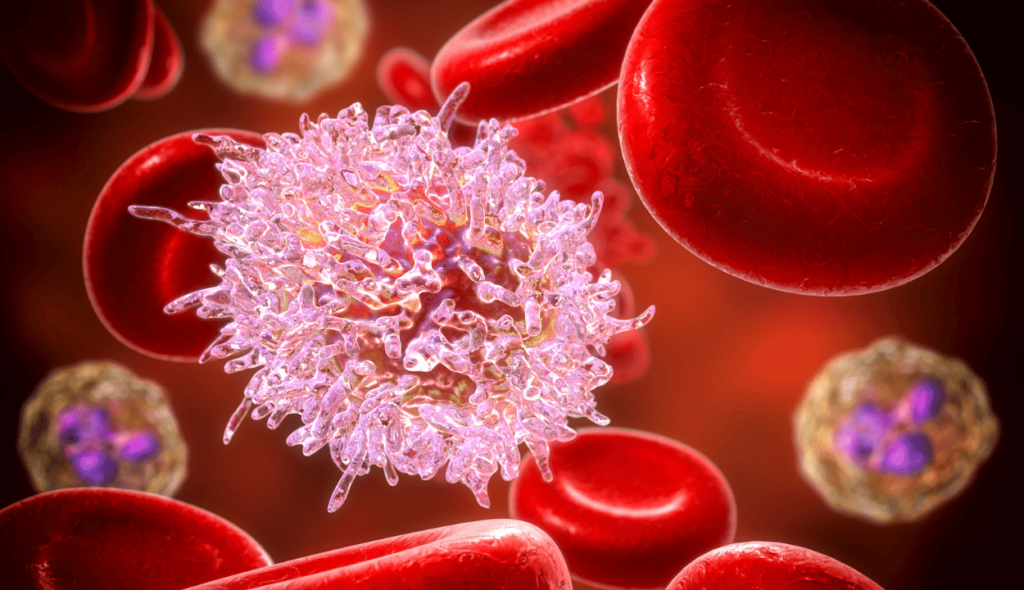
Hairy cell leukemia is an uncommon, slowly progressing blood cancer in which your bone marrow produces an excessive number of B cells (also known as lymphocytes), a type of white blood cell that fights infection.
Under a microscope, these extra B cells are aberrant and have a “hairy” appearance. Less healthy white blood cells, red blood cells, and platelets are created as the number of leukemia cells rises.
Men are more likely than women to have hairy cell leukemia, and middle-aged or older persons are the most frequently affected. The fact that hairy cell leukemia may never totally go away after years of remission following therapy makes it a chronic disease.
Symptoms of hairy cell leukemia
Hairy cell leukaemia may unintentionally be detected via a blood test for another illness or condition in patients who have no visible signs or symptoms of the disease.
Sometimes individuals with hairy cell leukemia exhibit signs and symptoms that are typical of a number of illnesses and ailments, including:
- A feeling of fullness in your abdomen that may make it uncomfortable to eat more than a little at a time
- Fatigue
- Easy bruising
- Recurring infections
- Weakness
- Weight loss
Diagnosis of hairy cell leukemia
Physical examination:
Your doctor can tell if your spleen is enlarged by feeling the oval-shaped organ on the left side of your upper belly. It may be unpleasant to eat because of an uncomfortable feeling of fullness in your abdomen brought on by an enlarged spleen.
Additionally, your doctor can look for swollen lymph nodes that may be home to leukemia cells.
Blood tests:
To keep track of the quantity of blood cells in your body, your doctor performs blood tests like the complete blood count.
Low numbers of red blood cells, white blood cells, and platelets are present in people with hairy cell leukemia. An further blood test known as a peripheral blood smear scans a sample of your blood for hairy cell leukemia cells.
Bone marrow biopsy:
A little sample of bone marrow from your hip area is taken during a bone marrow biopsy. This sample is used to check your healthy blood cells and look for hairy cell leukemia cells.
Computerized tomography (CT Scan):
A CT scan shows detailed images of the inside of your body. Your doctor may order a CT scan to detect enlargement of your spleen and your lymph nodes.
Treatment of hairy cell leukemia
A bone marrow biopsy involves taking a little sample of bone marrow from the hip region. Your healthy blood cells will be examined in this sample together with any potential hairy cell leukemia cells.
Chemotherapy
Two chemotherapy drugs are used in hairy cell leukemia:
Cladribine. Treatment for hairy cell leukemia typically begins with cladribine. You may receive either a continuous infusion of the drug or daily injections into a vein over several days.
Most people who receive cladribine experience a complete remission that can last for several years. If your hairy cell leukemia returns, you can be treated with cladribine again. Side effects of cladribine may include infection and fever.
- Pentostatin. Pentostatin (Nipent) causes remission rates similar to cladribine, but it’s given on a different schedule. People who take pentostatin receive infusions every other week for three to six months. Side effects of pentostatin may include fever, nausea and infection.
Biological treatments
Biological therapy attempts to make cancer cells more recognizable to your immune system. Once your immune system identifies cancer cells as intruders, it can set about destroying your cancer.
Two types of biological treatments are used in hairy cell leukemia:
Rituximab. Rituximab (Rituxan) is a monoclonal antibody approved to treat non-Hodgkin’s lymphoma and chronic lymphocytic leukemia, though it’s sometimes used in hairy cell leukemia.
If chemotherapy drugs haven’t worked for you or you can’t take chemotherapy, your doctor might consider rituximab. You doctor may also combine cladribine and rituximab. Side effects of rituximab include fever and infection.
Interferon. Currently, the role of interferon in hairy cell leukemia treatment is limited. You might receive interferon if chemotherapy hasn’t been effective or if you can’t take chemotherapy.
Most people experience partial remission with interferon, which is taken for a year. Side effects include flu-like symptoms, such as fever and fatigue.
Other drugs that target the immune system may be recommended if your cancer returns or if it doesn’t respond to standard treatments. Clinical trials are studying new biological therapies and targeted therapies for treating hairy cell leukemia.
Surgery
If your spleen ruptures or becomes huge and painful, surgery to remove it (a splenectomy) may be a possibility. While spleen removal won’t cure hairy cell leukaemia, it frequently returns blood counts to normal.
Although splenectomy is not frequently used to treat hairy cell leukemia, it might be advantageous in some circumstances. There is always a chance of bleeding and infection during surgery.
CAR T-Cell therapy for treatment of leukemia
Chimeric antigen receptor (CAR) T-cell therapy is a way to get immune cells called T cells (a type of white blood cell) to fight cancer by changing them in the lab so they can find and destroy cancer cells. CAR T-cell therapy is also sometimes talked about as a type of cell-based gene therapy, because it involves altering the genes inside T cells to help them attack the cancer.
This type of treatment can be very helpful in treating some types of cancer, even when other treatments are no longer working.
Apply for CAR T-Cell therapy
- Comments Closed
- June 28th, 2022



Latest Posts
- Targeting FGFR4 and CD276 with CAR T-cells demonstrates a strong antitumor impact against children rhabdomyosarcoma
- Disruption of CD5 on CAR T Cells Enhances the Effectiveness of Anti-Tumor Treatment
- The future of gene therapy: What to expect in the next decade?
- Unlocking the genetic code: The future of gene therapy for genetic disorders
- CRISPR and gene editing: Revolutionizing gene therapy
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (56)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (787)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (95)
- Cervical cancer (41)
- Chemotherapy (36)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (19)
- Endometrial cancer (9)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (1)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (47)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (44)
- Liver cancer (94)
- Lung cancer (65)
- Lymphoma (44)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (22)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (11)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (7)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (746)
- Treatment in China (646)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview