Blood cancer
What is blood cancer?
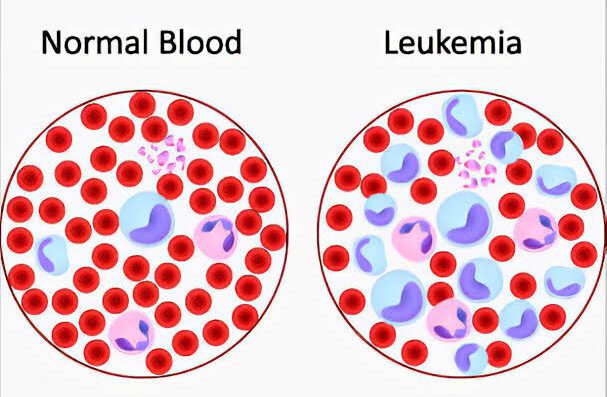
The majority of blood cancers, also referred to as hematologic cancers, begin in the bone marrow, where blood is made. Blood cancers arise when irregular blood cells start to develop out of control, interrupting the function of normal blood cells that combat infection and create new blood cells. The development and function of your blood cells are impaired by blood cancers. Most of these cancers start where blood is formed in your bone marrow. Stem cells grow and turn into three blood cell forms in your bone marrow: red blood cells, white blood cells, or platelets. In most blood cancers, uncontrolled growth of an irregular form of blood cell prevents the normal blood cell production method. These abnormal blood cells, or cancer cells, stop the blood from performing many of its functions, such as preventing severe bleeding or fighting off infections.
What are the types of blood cancer?
There are three main types of blood cancers:
- Leukemia : The rapid development of irregular white blood cells causes a form of cancer that is located in your blood and bone marrow. The large number of white blood cells that are defective are unable to combat infection and hinder the bone marrow’s capacity to produce red blood cells and platelets.
- Lymphoma : It is a form of cancer of the blood that affects the lymphatic system, which removes the body from excess fluids and generates immune cells. Lymphocytes are an infection-fighting type of white blood cells. In your lymph nodes and other tissues, dysfunctional lymphocytes become lymphoma cells, which grow and accumulate. These cancerous cells impair the immune system over time.
- Myeloma : This is plasma cell cancer. Plasma cells are white blood cells that contain antibodies in your body that combat disease and infection. Myeloma cells inhibit normal antibody development, leaving the immune system of your body compromised and vulnerable to infection.
Check : Cost of blood cancer treatment in India
Who are at risk of blood cancer?
Blood cancer risk factors are not well known, but blood cancers are believed to arise from a combination of genetic and environmental factors. Smoking, exposure to radiation, and exposure to chemicals such as benzene (a frequently used industrial chemical) have also been associated with an increased risk of some forms of blood cancers. Some risk factors for developing lymphomas and leukemias are Epstein-Barr virus, HIV and human T-cell lymphoma/leukemia virus infections.
What are the symptoms of blood cancer?
Symptoms of blood cancer vary by disease but typically include the following:
- Fever
- Chills
- Fatigue
- Weakness
- Bone and joint pain
- Weight loss
The swelling of lymph nodes, liver and spleen are also common, and anemia can occur in some blood cancers.
Check : Cost of blood cancer treatment in Israel
How is blood cancer diagnosed?
- Leukemia : A full blood count (CBC) examination will be administered by your doctor, and will detect elevated white blood cell levels compared to red blood cells and platelets.
- Lymphoma : A biopsy, which extracts a small portion of the tissue to be studied under a microscope, may need to be performed by your doctor. Your doctor can also prescribe an X-ray, CT or PET scan to detect enlarged lymph nodes in some cases.
- Myeloma: In order to detect chemicals or proteins formed as a function of myeloma growth, your doctor will order a CBC test or other blood or urine tests. Bone marrow biopsy, X-ray, MRI, PET, and CT scans can be used in certain cases to confirm the existence and extent of myeloma propagation.
Check : Cost of blood cancer treatment in South Korea
What are the treatment options in blood cancer?
Treatment depends on the form of blood cancer, your age, how rapidly the cancer progresses, and whether the cancer has spread to other areas of the body.
Since blood cancer therapies have advanced significantly over the past few decades, several forms of blood cancers are now highly treatable. The following are typical treatments:
- Chemotherapy : In order to kill and avoid the development of cancer cells, anticancer drugs are introduced to the body (via injection into the vein or often by taking a pill).
- Radiation therapy : To destroy cancer cells, this type of cancer treatment uses high-energy rays.
- Targeted therapies : Drugs that directly destroy malignant blood cells are used in this type of cancer treatment, without damaging normal cells. Most commonly targeted treatments are used to treat leukemia.
- Bone marrow / Stem cell transplantation : In order to help resume safe blood production after treatment to remove malignant blood cells, healthy stem cells may be injected into the body.
- Cancer Surgery : In order to cure certain lymphomas, this therapy includes removing the infected lymph nodes.
- Immunotherapy :The immune system is triggered by this procedure to directly destroy cancer cells.
Check : Cost of blood cancer treatment in Thailand
Take second opinion on blood cancer treatment
- Comments Closed
- July 5th, 2020



Latest Posts
- Targeting FGFR4 and CD276 with CAR T-cells demonstrates a strong antitumor impact against children rhabdomyosarcoma
- Disruption of CD5 on CAR T Cells Enhances the Effectiveness of Anti-Tumor Treatment
- The future of gene therapy: What to expect in the next decade?
- Unlocking the genetic code: The future of gene therapy for genetic disorders
- CRISPR and gene editing: Revolutionizing gene therapy
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (56)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (787)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (95)
- Cervical cancer (41)
- Chemotherapy (36)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (19)
- Endometrial cancer (9)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (1)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (47)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (44)
- Liver cancer (94)
- Lung cancer (65)
- Lymphoma (44)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (22)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (11)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (7)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (746)
- Treatment in China (646)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview