Acute lymphoblastic leukemia
What is acute lymphoblastic leukemia?
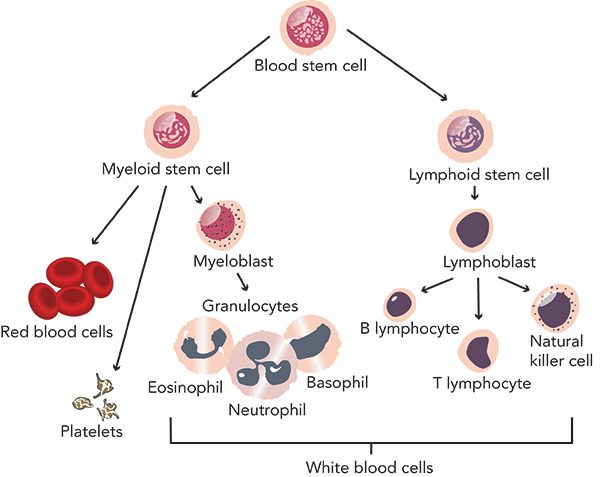
Acute lymphocytic leukemia is also referred to as acute lymphoblastic leukemia (ALL). “Acute” means that leukemia can develop rapidly, and is likely to be lethal within a couple of months if not treated. “Lymphocytic” means that it produces a type of white blood cell from early (immature) types of lymphocytes.
In the bone marrow, ALL begins (the soft inner part of certain bones, where new blood cells are made). Very commonly, blood is infiltrated very rapidly by leukemia cells. They can also spread to other parts of the body often, including the lymph nodes, liver, spleen, brain and spinal cord, central nervous system, and testicles (in males). In these organs, some cancers can also begin and then spread to the bone marrow, but these cancers are not leukemia.
A type of blood and bone marrow cancer, the spongy tissue inside the bones where blood cells are formed, is acute lymphocytic leukemia (ALL).
In acute lymphocytic leukemia, the term “acute” comes from the fact that the disease progresses quickly and produces immature blood cells instead of mature ones. In acute lymphocytic leukemia, the term “lymphocytic” refers to the white blood cells called lymphocytes affected by Everything. Acute lymphocytic leukemia is often referred to as acute lymphoblastic leukemia.
The most common form of cancer in children is acute lymphocytic leukemia, and therapies result in a strong chance of a cure. There can also be acute lymphocytic leukemia in adults, but the likelihood of a cure is significantly diminished.
Causes and Risk Factors for Acute Lymphoblastic Leukemia
Doctors are unsure of what triggers the bulk of ALL incidents. But studies have found that certain items could increase your risk, including:
- Contact with high levels of radiation to treat other types of cancer
- Contact with chemicals such as benzene, a solvent used in oil refineries and other industries and found in cigarette smoke; and some cleaning products, detergents, and paint strippers
- Infection with the human T-cell lymphoma/leukemia virus-1 (HTLV-1) or the Epstein-Barr virus (EBV), mostly outside the U.S.
- Having a medical condition that’s tied to your genes, such as Down syndrome
- Being white
- Being male
Symptoms of acute lymphocytic leukemia (ALL)
Signs and symptoms of acute lymphocytic leukemia may include:
- Bleeding from the gums
- Bone pain
- Fever
- Frequent infections
- Frequent or severe nosebleeds
- Lumps caused by swollen lymph nodes in and around the neck, underarm, abdomen or groin
- Pale skin
- Shortness of breath
- Weakness, fatigue or a general decrease in energy
Causes of acute lymphocytic leukemia (ALL)
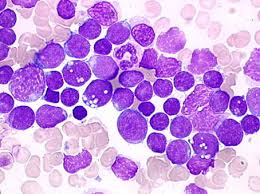
When a bone marrow cell produces errors in its DNA, acute lymphocytic leukemia occurs. When a healthy cell usually stops dividing and ultimately dies, the errors tell the cell to continue developing and dividing. The development of blood cells becomes irregular when this occurs. The bone marrow generates immature cells that turn into lymphoblasts called leukemic white blood cells. These dysfunctional cells cannot function properly, and healthy cells can be built up and crowded out.
What triggers the DNA mutations which can lead to acute lymphocytic leukemia is not clear. Yet most cases of acute lymphocytic leukemia are not hereditary, doctors have found.
Risk factors for acute lymphocytic leukemia (ALL)
The following are factors that can raise the risk of acute lymphocytic leukemia:
Treatment for past cancer : There could be an elevated risk of developing acute lymphocytic leukemia in children and adults who have had some forms of chemotherapy and radiation therapy for other kinds of cancer.
Radiation sensitivity : There is an elevated risk of developing acute lymphocytic leukemia in individuals who are exposed to extremely high levels of radiation, such as survivors of a nuclear reactor accident.
Having inherited disorders: An elevated risk of acute lymphocytic leukemia is associated with some genetic conditions, such as Down syndrome.
Getting an all-ALL brother or sister: People with acute lymphocytic leukemia who have a sibling, even a twin, have an increased chance of developing Both.
Acute Lymphoblastic Leukemia Diagnosis
Your doctor will ask about your symptoms and medical history. They’ll do a physical exam to look for swollen lymph nodes, bleeding and bruising, or signs of infection.
If your doctor suspects leukemia, they may do tests, including:
- Blood tests. A complete blood count (CBC) shows how many of each type of blood cell you have. A peripheral blood smear checks for changes in how your blood cells look.
- Bone marrow tests. Your doctor will put a needle into a bone in your chest or hip and take out a sample of bone marrow. A specialist will look at it under a microscope for signs of leukemia.
- Imaging tests. X-rays, CT scans, or ultrasounds can tell your doctor whether the cancer has spread.
- Spinal tap. This is also known as a lumbar puncture. Your doctor will use a needle to take a sample of fluid from around your spinal cord. A specialist can look at it to see if the cancer has reached your brain or spinal cord.
Your doctor can also monitor for changes in your chromosomes in your blood or bone marrow, or check for cancer cell markers. The findings will teach them all about the type of leukemia that you have and help prepare the care for them.
Acute Lymphoblastic Leukemia Treatment
Treatment happens in two parts: induction therapy, to put you in remission, and post-remission therapy.
You may have more than one type of treatment. These include:
- Chemotherapy. You might take a mix of drugs that kill or slow cancer cells, usually over a couple of years.
- Targeted therapy. Some drugs target specific parts of cancer cells and tend to have fewer or milder side effects than chemotherapy. They include dasatinib (Sprycel), imatinib (Gleevec), nilotinib (Tasigna), and ponatinib (Iclusig).
- Radiation therapy. Your doctor might use high-energy radiation to kill cancer cells if they’ve reached your brain or bone or before you have a stem cell transplant.
- Immunotherapy. These drugs boost your immune system to kill or slow the growth of cancer cells. They include blinatumomab (Blincyto) and inotuzumab ozogamicin (Besponsa).
- A stem cell transplant. After high doses of chemotherapy and possibly radiation, you get stem cells that will grow into healthy blood cells. They might be your own or come from a donor. If you can’t handle high doses of chemotherapy and radiation, you might get lower doses with a “mini-transplant.”
About 80% to 90% of adults reach remission after treatment. For about 30% to 40%, the cancer doesn’t return. But many relapse, meaning the disease returns.
You’ll need post-remission therapy to keep the cancer from coming back. This involves cycles of treatment over 2 to 3 years. It aims to rid your body of leukemia cells.
The FDA has also approved a form of treatment called CAR T-cell therapy. It uses some of your own immune cells, called T cells, to treat your cancer. Doctors take the cells out of your blood and add genes to them. The new T cells are better able to find and kill cancer cells. CAR T Cell therapy in China has gained a lot of attention because of the number of clinical trials running across the big hospitals.
- Comments Closed
- September 2nd, 2020



Latest Posts
- LungVax: Lung cancer vaccine
- Successful CRISPR Gene Therapies in Practice: Case Studies
- Gamma Delta (γδ) T cells as a potential treatment for glioblastoma
- World-first lung cancer vaccine trials started in seven countries
- Lazertinib with amivantamab-vmjw is approved by the USFDA for non-small lung cancer
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (58)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (790)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (104)
- Cervical cancer (41)
- Chemotherapy (37)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (20)
- Endometrial cancer (10)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (2)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (48)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (45)
- Liver cancer (94)
- Lung cancer (69)
- Lymphoma (46)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (23)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (12)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (8)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (747)
- Treatment in China (647)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview