Fanconi anemia
Fanconi anemia (FA)
Fanconi anaemia (FA) is a rare genetic disease marked by a variety of physical defects, bone marrow loss, and an increased risk of malignancy. FA can be caused by flaws (mutations) in one of at least 15 distinct genes, according to research. The proteins produced by these genes build a cellular “machine” that helps blood stem cells and other cells in the body detect and repair damaged DNA (a normal, daily occurrence). This DNA repair is delayed in FA. As a result, damaged DNA accumulates in blood stem cells (in the bone marrow), and they die.
FA is usually discovered between the ages of one and ten years. There have, however, been cases identified in adults. FA affects both men and women equally. It has been found in people of various ethnicities. Researchers are still cloning and characterising the genes that cause FA, making significant advances in the diagnosis and understanding of the illness.
What causes Fanconi anemia?
Individuals with FA have chromosomes that are unable to repair deoxyribonucleic acid (DNA) damage, allowing them to easily break and rearrange (chromosome instability). DNA is the carrier of the genetic code, and it is damaged on a daily basis. Damage to DNA is usually repaired in most people. Individuals with FA, on the other hand, experience more breakage and rearrangements, and their bodies are delayed or fail to heal the damage.
FA is caused by mutations in at least 18 genes. When DNA damage occurs, the proteins produced by these genes function together in a pathway known as the FA pathway, which kicks in when DNA damage occurs. The FA route transports specific proteins to the site of DNA damage, allowing it to be repaired and copied (replicated). The FA core complex is made up of eight proteins that activate two genes to produce the proteins FANCD2 and FANCI. When these two proteins are activated, DNA repair proteins are drawn to the location of DNA damage.
Mutations in one of three genes, FANCA, FANCC, or FANCG, cause 80% to 90% of instances of FA. These genes give instructions on how to make FA core complex components. Any of the many genes connected with the FA core complex can be mutated, rendering the complex inoperable and disrupting the overall FA pathway. When this route is disrupted, DNA damage accumulates, which can result in aberrant cell death or proliferation. A reduction in blood cells and physical abnormalities linked with FA come from cell death. Acute myeloid leukaemia and other cancers can be caused by uncontrolled cell growth.
FA is inherited in the majority of cases as an autosomal recessive trait. When an individual receives two copies of a defective gene for the same trait, one from each parent, recessive genetic diseases emerge. If a person receives one normal gene and one illness gene, he or she will be a carrier for the disease but will not normally show symptoms. With each pregnancy, there is a 25% chance that two carrier parents will both pass the mutated gene and have an afflicted child. With each pregnancy, there is a 50% chance of having a child who is a carrier like the parents. A child has a 25% chance of inheriting normal genes from both parents. Males and females are equally at risk.
Close relatives (consanguineous) have a larger likelihood of carrying the same faulty gene than unrelated parents, increasing the risk of having children with a recessive genetic condition.
BRCA2, BRIP1, FANCB, FANCD2, FANCE, FANCF, FANCI, ERCC4, FANCL, FANCM, PALB2, RAD51C, SLX4, and UBE2T all have mutations that induce FA and are inherited in an autosomal recessive way.
The FANCB gene is found on the X chromosome and accounts for fewer than 1% of all FA cases. This FA gene is inherited as a recessive X-linked characteristic.
Males are more likely to get X-linked genetic illnesses, which are caused by a faulty gene on the X chromosome. Females that carry a mutation on one of their X chromosomes are carriers for the illness. Because females have two X chromosomes, one of which carries the mutated gene, carrier females normally do not show symptoms. Males have one X chromosome, which they inherit from their mother, and if that chromosome contains a mutated gene, the male will suffer the disease. With each pregnancy, female carriers of an X-linked ailment have a 25% chance of having a carrier daughter like themselves, a 25% chance of having a non-carrier daughter, a 25% risk of having a son affected by the disease, and a 25% chance of having an unaffected son. If a man with an X-linked illness is able to reproduce, the changed gene will be passed down to all of his daughters who are carriers. Because males usually convey their Y chromosome to male progeny instead of their X chromosome, a male cannot pass an X-linked gene to his sons.
Autosomal dominant FA is caused by mutations in the RAD51 gene. When only one copy of a defective gene is required to induce a disease, it is known as a dominant genetic illness. The faulty gene can be inherited from either parent or caused by a new mutation (gene alteration) in the affected person. Each pregnancy has a 50% chance of transferring the faulty gene from an affected parent to an offspring. Males and females are equally at risk. To date, all people who have FA because of a RAD51 gene mutation have a spontaneous (de novo) genetic mutation in their egg or sperm cell. In such cases, the illness is not passed down from one generation to the next.
Sings and symptoms of Fanconi anemia
FA symptoms differ from one person to the next. Physical abnormalities, bone marrow loss, and a higher risk of cancer are among the symptoms identified. Physical anomalies usually show up in early childhood, although in certain situations, diagnoses are made later in life. Between the ages of 6 and 8, issues with blood production are common. Bone marrow failure strikes the majority of people at some point, though the rate of occurrence and age of onset differ. Whether or whether they have earlier blood problems, patients who live into adulthood are more likely to acquire head and neck, gynecologic, and/or gastrointestinal cancer at a considerably younger age than the overall population.
Physical Abnormalities
At least 60% of individuals affected with FA are born with at least one physical anomaly. This may include any of the following:
-short stature
-thumb and arm anomalies: an extra or misshaped or missing thumbs and fingers or an incompletely developed or missing radius (one of the forearm bones)
-skeletal anomalies of the hips, spine, or ribs
-kidney structural problems
-skin pigmentation (called café au lait spots)
-small head
-small, crossed, or widely spaced eyes
-low birth weight
-gastrointestinal difficulties
-small reproductive organs in males
-defects in tissues separating chambers of the heart
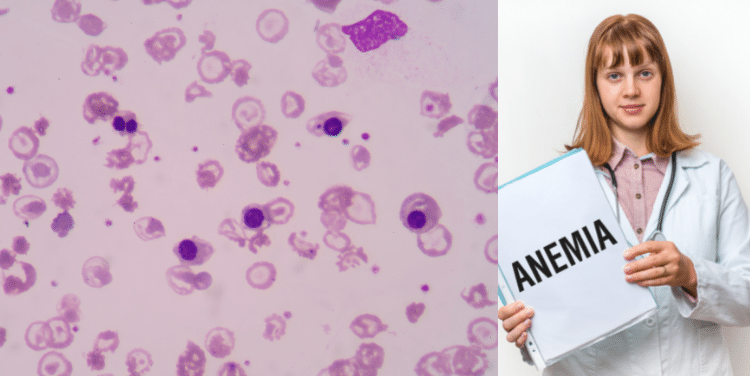
Individuals with anemia may experience tiredness, increased need for sleep, weakness, lightheadedness, dizziness, irritability, headaches, pale skin color, difficulty breathing, and cardiac symptoms.
There may be excessive bruising following minimal injury and spontaneous bleeding from the mucous membranes, especially those of the gums and nose.
Bone marrow failure
The spongy substance found in the core of the long bones of the body is called bone marrow. Hematopoietic stem cells are produced in the bone marrow and expand to become red blood cells (erythrocytes), white blood cells (leukocytes), and platelets. The cells are released into the bloodstream to complete their jobs as they travel throughout the body. Red blood cells carry oxygen around the body, white blood cells combat infections, and platelets help the body stop bleeding by forming clots.
Progressive bone marrow failure usually manifests by the age of ten, and is accompanied by low platelet or white blood cell counts. Bone marrow failure is predicted to be the first major event in more than half of people between the ages of 40 and 50.
Affected individuals develop low levels of all the cellular elements of the bone marrow- red and white blood cells and platelets- which can lead to the following:
-low level of circulating red blood cells – anemia
-low level of white blood cells – leukopenia
-low level of neutrophils (a type of white blood cell) – neutropenia
-low level of platelets – thrombocytopenia
Increased Risk of Malignancy
Individuals with FA have a higher risk than the general population of developing certain forms of cancer including acute myeloid leukemia and specific solid tumors. Affected individuals may are at extremely high risk of developing cancer affecting the head and neck region, gastrointestinal tract, esophagus or gynecologic regions. Most of these are a specific form of cancer, known as squamous cell carcinoma. FA patients whose bone marrow failure is treated with male hormones (called “androgens”) have in increased risk of liver tumors.
In approximately 30 percent of cases associated with cancer, the development of malignancy precedes a diagnosis of FA.
Diagnosis of Fanconi anemia
A thorough clinical evaluation, a detailed patient history, identification of distinctive symptoms, and a variety of specialist testing are used to diagnose FA.
At this time, the only definite diagnostic for FA is a chromosome breakage test, which involves treating some of the patient’s blood cells in a test tube with a substance that crosslinks DNA. Normal cells can repair most of the damage and are unaffected, whereas FA cells have significant chromosome breakage. DEB (diepoxybutane) and MMC (methoxymethylcellulose) are two compounds typically utilised in this test (mitomycin C). These tests can be done on chorionic villi or amniotic fluid cells during pregnancy.
The levels of red and white blood cells, as well as platelets, can be determined through blood testing. X-rays can identify the presence and extent of skeletal deformities as well as structural abnormalities within the body.
Many cases of FA are undiagnosed or go undiagnosed for long periods of time. Any newborn born with the thumb and arm anomalies indicated above should be suspected of FA and examined. Even if no other problems are evident, anyone developing aplastic anaemia at any age should be tested for FA. Any patient with a history of tobacco or alcohol use who develops squamous cell carcinoma of the head and neck, gastrointestinal, or gynecologic system at a young age should be tested for FA. Many FA sufferers have no additional symptoms. Standard chemotherapy and radiation treatments may be hazardous to FA patients, hence testing for FA is required before considering stem cell transplantation for aplastic anaemia or cancer treatment.
All 18 genes linked to FA can be tested using molecular genetics. Complementation testing is often performed initially to determine which FA gene has been altered. The specific mutation in that gene can subsequently be determined using sequence analysis of the applicable gene. If a mutation is not found, clinical deletion/duplication analysis for the genes linked to FA is available.
Targeted mutation analysis is available for the common Ashkenazi Jewish FANCC mutation.
Clinical Testing/ Work Up
To establish the extent of disease in an individual diagnosed with FA, the following evaluations are recommended as needed:
-Ultrasound examination of the kidneys and urinary tract
-Formal hearing test
-Developmental assessment (particularly important for toddlers and school-age children)
-Referral to an ophthalmologist, otolaryngologist, endocrinologist, hand surgeon, gynecologist (for females as indicated), gastroenterologist, urologist, dermatologist, ENT surgeon, genetic counselor
-Evaluation by a hematologist, to include complete blood count, fetal hemoglobin, and bone marrow aspirate for cell morphology and chromosome study (cytogenetics), as well as biopsy for cellularity
-HLA typing of the affected individual, siblings, and parents for consideration of hematopoietic stem cell transplantation
-Full blood typing
-Blood chemistries (assessing liver, kidney, thyroid, lipids, and iron status).
Treatment of Fanconi Anemia
The treatment for FA is tailored to the exact symptoms that each person exhibits. Treatment may necessitate the collaboration of a group of professionals. Pediatricians, surgeons, cardiologists, kidney specialists (nephrologists), urologists, gastroenterologists, hearing specialists (audiologists and otolaryngologists), eye specialists, and other health care professionals may be required to plan an affected individual’s treatment in a systematic and comprehensive manner.
-Androgen (male hormone) administration: Androgens improve the blood counts in approximately 50% of individuals with FA. The earliest response is seen in red cells, with increase in hemoglobin generally occurring within the first month or two of treatment. Responses in the white cell count and platelet count are variable. Platelet responses are generally incomplete and may not be seen before several months of therapy. Improvement is generally greatest for the red cell count. Resistance to therapy may develop over time.
-Hematopoietic growth factors: Granulocyte colony-stimulating factor (G-CSF) may improve the neutrophil count in some individuals. It is usually used only for support during intercurrent illnesses.
-Hematopoietic stem cell transplantation (HSCT): the only curative therapy for the hematologic manifestations of FA. Donor stem cells may be obtained from bone marrow, peripheral blood, or cord blood.
–Cancer treatment: Treatment of malignancies is challenging secondary to the increased toxicity associated with chemotherapy and radiation in FA. Care should be obtained from centers experienced in the treatment of FA patients.
Surgery may be necessary to correct skeletal malformations such as those affecting the thumbs and forearm bones, cardiac defects, and gastrointestinal abnormalities such as tracheoesophageal fistula or esophageal atresia, as well as anal atresia.
Certain chemicals may increase the risk of chromosomal breakage in individuals with FA and should be avoided whenever possible. These chemicals include tobacco smoke, formaldehyde, herbicides, and organic solvents such as gasoline or paint thinner.
Genetic counseling is recommended for affected individuals and their families.
- Comments Closed
- February 4th, 2022



Latest Posts
- Targeting FGFR4 and CD276 with CAR T-cells demonstrates a strong antitumor impact against children rhabdomyosarcoma
- Disruption of CD5 on CAR T Cells Enhances the Effectiveness of Anti-Tumor Treatment
- The future of gene therapy: What to expect in the next decade?
- Unlocking the genetic code: The future of gene therapy for genetic disorders
- CRISPR and gene editing: Revolutionizing gene therapy
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (56)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (787)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (95)
- Cervical cancer (41)
- Chemotherapy (36)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (19)
- Endometrial cancer (9)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (1)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (47)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (44)
- Liver cancer (94)
- Lung cancer (65)
- Lymphoma (44)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (22)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (11)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (7)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (746)
- Treatment in China (646)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview