Vaginal cancer
Vaginal cancer
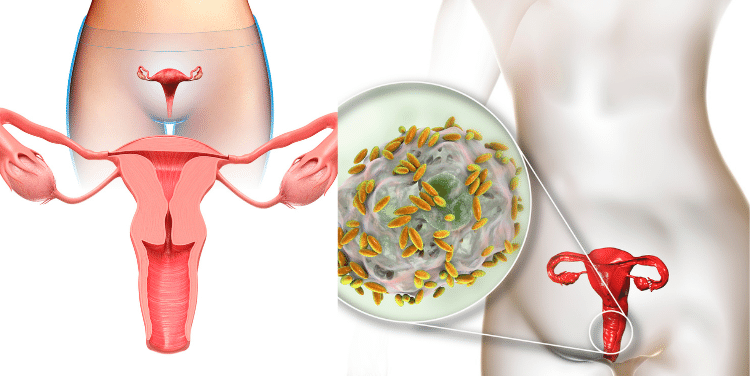
The abnormal proliferation of malignant (cancerous) cells in the vagina is known as vaginal cancer. Squamous cell carcinomas account for roughly 85 percent of vaginal malignancies. These grow in the vaginal “skin” (epithelial lining). They are frequently located around the cervix in the upper region of the vagina. They develop from precancerous spots called vaginal intraepithelial neoplasia over a long period of time (VAIN).
Adenocarcinomas account for 5-10% of vaginal cancers. These originate in glandular tissues. Clear cell adenocarcinoma is a subtype of these cancers. These are especially common in young women whose moms used the hormone diethylstilbestrol (DES) while they were pregnant with them.
Melanomas (2-3 percent), which appear in the lower or outside section of the vagina, sarcomas (2-3 percent), and even rarer kinds such small cell, lymphoma, and carcinoid cancer are all rare types of vaginal cancer. This article does not include these subtypes.
Most vaginal malignancies are metastases, not “primary” tumours (tumours that begin in the vagina) (cancers that have spread from another site in the body to the vagina). This can be caused by a tumour growing directly into the vagina (for example, from the endometrium, rectum, or bladder) or by a tumour migrating through the bloodstream or lymph system from a distant place (for example, from the breast or ovary).
Vaginal cancer is a rare type of cancer that starts in the vagina. It accounts for about 2 percent trusted Source of female genital cancers, the National Cancer Institute (NCI) estimates.
There are several main types of vaginal cancer, including:
- Squamous cell. This type of cancer starts in the vaginal lining and develops slowly. It accounts for approximately 9 out of 10Trusted Source vaginal cancer cases, according to the American Cancer Society (ACS).
- Adenocarcinoma. This type of cancer starts in the vaginal gland cells. It’s the second most common type of vaginal cancer and is most prevalent in women over 50.
- Melanoma. As with the more common skin cancer type of melanoma, this type of cancer starts in the cells that give skin color.
- Sarcoma. This starts in the vaginal walls and accounts for only a small percentage of vaginal cancers.
In early stages, vaginal cancer treatment has a high success rate.
Risk factors for vaginal cancer
A risk factor is something that enhances your chances of contracting a disease. Having a risk factor does not guarantee that you will develop cancer; similarly, not having a risk factor does not guarantee that you will remain cancer-free. If you think you could be at danger, talk to your doctor. The following are some of the risk factors for vaginal cancer:
- Being 60 years or older.
- Having a human papilloma virus (HPV) infection. Squamous cell carcinoma (SCC) of the vagina is linked to HPV infection and has many of the same risk factors as SCC of the cervix.
- Being exposed to DES while in the mother’s womb. In the 1950s, the drug DES was given to some pregnant women to prevent miscarriage (premature birth of a fetus that cannot survive). This is linked to a rare form of vaginal cancer called clear cell adenocarcinoma. The rates of this disease were highest in the mid-1970s, and it is extremely rare now.
- Having had a hysterectomy for tumors that were benign (not cancer) or cancer.
Signs and symptoms of vaginal cancer
Painless vaginal bleeding that is unrelated to menstrual cycles is the most prevalent symptom. Bleeding after a sexual encounter could be a symptom of vaginal cancer. Vaginal bleeding in a postmenopausal woman is alarming and should be addressed as soon as possible. Vaginal discharge and painful sexual intercourse are two more possible signs. Due to tumour invasion into the rectum, more advanced vaginal malignancies may also cause digestive symptoms such as blood in the stool, painful bowel movements, or constipation. Vaginal malignancies can sometimes move to the bladder, making urination uncomfortable or difficult.
The most common is abnormal vaginal bleeding.
This includes bleeding after:
- menopause
- bleeding during or after sex
- bleeding in between menstruation
The bleeding may also be heavier or go on for longer trusted Source than usual.
Other symptoms include:
- vaginal discharge that’s watery, smells, or is bloodstained
- painful or frequent urination
- pelvic pain, especially during sex
- a lump or mass in the vagina
- constant itchiness in the vagina
- constipation
- blood in stool or urine
- back pain
- swollen legs
- fistulas, in later stage cancer
Diagnosis of vaginal cancer
A pelvic examination is one of the most crucial measures in examining a lady with a gynecologic issue. A healthcare professional (HCP) examines the uterus, ovaries, fallopian tubes, and vagina by feeling the areas with their hands and looking at visible areas during this examination. Any anomalies in the bladder and rectum should be checked as well. This may necessitate a cystoscopy or proctosigmoidoscopy, in which a camera is used to inspect the inside of the bladder and rectum/bowel, respectively.
Radiology tests, such as CT scans, MRIs, and PET scans, can be used to check for enlarged lymph nodes, kidney/bladder problems, liver abnormalities, and other places where cancer could spread (metastasis).
It is recommended that a Pap test be performed. A instrument scrapes the exterior of the cervix and vagina during a Pap test. The samples are examined under a microscope and HPV testing is performed. Even if your doctor suspects you of having vaginal cancer, a Pap smear is necessary to rule out cervical cancer. Cervical cancer screening using a Pap smear can detect up to 20% of vaginal cancers.
It is possible to perform a colposcopy. A device with binocular magnifying lenses is inserted into the vagina to look at the cervix and the inside of the vagina during colposcopy. Biopsies of worrisome regions on the cervix and/or along the vaginal walls should be taken and sent to a lab for microscopic examination. Applying a dilute solution of acetic acid to any suspect spots should be examined. Normally, abnormal spots turn white, making them easier to spot and biopsy.
Stages of vaginal cancer
Stage I
In stage I, cancer is only found in the vaginal wall.
Stage II
In stage II, cancer has spread through the wall of the vagina to the tissue around the vagina. Cancer has not spread to the wall of the pelvis.
Stage III
In stage III, cancer has spread to the wall of the pelvis.
Stage IV
Stage IV is divided into stage IVA and stage IVB:
- Stage IVA: Cancer may have spread to one or more of the following areas:
- The lining of the bladder.
- The lining of the rectum.
- Beyond the area of the pelvis that has the bladder, uterus, ovaries, and cervix.
- Stage IVB: Cancer has spread to parts of the body that are not near the vagina, such as the lung or bone.
The cancer may come back in the vagina or in other parts of the body.
The vaginal cancer is staged once the diagnosis has been verified. Staging aids the practitioner in determining which therapy options are best for each patient. Vaginal cancer is staged depending on the results of the physical exam, radiological testing, and any biopsies, unlike many cancer forms that are not staged until after surgery. Because many women with vaginal cancer will not have surgery as their first treatment, this is referred to as “clinical staging.”
Vaginal cancer is divided into four stages to help guide treatment and provide insight into prognosis. The FIGO system is the staging system for vaginal cancer (International Federation of Gynecologists and Obstetricians). The TNM system is also used by healthcare providers (also called tumour – node – metastasis system). This system specifies the tumor’s size and local invasiveness (T), the presence of lymph nodes (N), and whether the tumour has moved to other parts of the body (M). This is then interpreted as a stage ranging from I (limited disease) to IV (advanced disease), with I (one) representing more limited disease and IV (four) denoting more advanced disease.
Treatment of vaginal cancer
The most common treatments are surgery, radiation therapy, and chemotherapy. These can be employed as single-mode or multi-modal therapy.
There is no such thing as a “standard” treatment for vaginal cancer, and each woman’s treatment should be tailored to her specific situation. Treatment options should include the patient’s disease stage, age, medical history, and personal preferences, among other factors.
Surgery might be used to remove part or all of the vaginal tissue (called vaginectomy). Small lesions in the upper vaginal area are frequently the best candidates for surgery. Hysterectomy and excision of the vaginal and local lymph nodes are among the procedures that may be performed. Radiation therapy is a viable alternative to surgery in many circumstances. Chemotherapy (sometimes known as neoadjuvant chemotherapy) may be used to decrease the tumour before it is removed in some circumstances. Vaginal reconstruction may be an option for women who have had a vaginectomy. A vaginal canal is created by the surgeon using a skin or muscle flap taken from another part of the body.
High-energy rays are used in radiation therapy to eliminate cancer cells. It is the therapy of choice for the majority of patients with invasive vaginal cancer, particularly those with stage II or higher illness. It can be given as external beam radiation (from a machine), brachytherapy (using radioactive “seeds” supplied through thin plastic tubes directly into the diseased area), or a mix of the two. Small malignancies in the upper section of the vaginal canal can sometimes be treated with brachytherapy alone. When patients experience a recurrence following radiation, surgery is usually the chosen option.
Chemotherapy is a treatment that uses drugs to kill cancer cells. There are no randomised clinical trial data supporting the use of chemotherapy and radiation for vaginal cancer due to the disease’s rarity. Many HCPs prescribe concurrent radiation and cisplatin-based chemotherapy for high-risk vaginal cancer patients, based on multiple studies in cervical cancer that indicate better results with the combination compared to radiation alone. Carboplatin, fluorouracil, paclitaxel, and docetaxel are some of the additional chemotherapy drugs used to treat vaginal cancer. Chemotherapy can also be used to manage (rather than cure) recurrent or widespread illness.
Take second opinion on vaginal cancer treatment
- Comments Closed
- January 12th, 2022



Latest Posts
- Targeting FGFR4 and CD276 with CAR T-cells demonstrates a strong antitumor impact against children rhabdomyosarcoma
- Disruption of CD5 on CAR T Cells Enhances the Effectiveness of Anti-Tumor Treatment
- The future of gene therapy: What to expect in the next decade?
- Unlocking the genetic code: The future of gene therapy for genetic disorders
- CRISPR and gene editing: Revolutionizing gene therapy
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (56)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (787)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (95)
- Cervical cancer (41)
- Chemotherapy (36)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (19)
- Endometrial cancer (9)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (1)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (47)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (44)
- Liver cancer (94)
- Lung cancer (65)
- Lymphoma (44)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (22)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (11)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (7)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (746)
- Treatment in China (646)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview