Gastrointestinal stromal tumors
Gastrointestinal stromal tumors
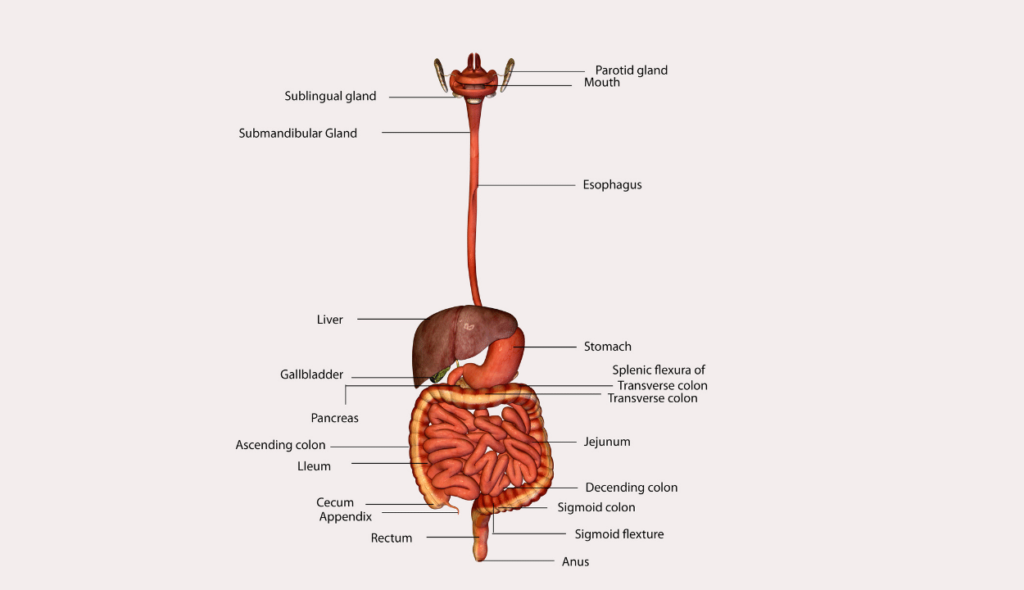
Gastrointestinal stromal tumors (GISTs) begin in very early stages in the interstitial cells of Cajal, a specific type of cell found in the GI tract wall (ICCs). Because they tell the GI tract’s muscles to contract to transport food and liquid along, ICCs are frequently referred to as the “pacemakers” of the digestive system.
In the stomach, more than half of GISTs begin. GISTs can begin anywhere throughout the GI tract, unlike most other cancers, which often begin in the small intestine. A tiny percentage of GISTs begin outside the GI tract in surrounding regions such the peritoneum or the omentum, which is a fatty layer that drapes over the abdominal organs like an apron (the thin lining over the organs and walls inside the abdomen).
Some GISTs seem to be much more likely than others to grow into other areas or spread to other parts of the body. Doctors look at certain factors to help tell whether a GIST is likely to grow and spread quickly, such as:
- The size of the tumor
- Where it’s located in the GI tract
- How fast the tumor cells are dividing.
Symptoms of GSIT
The stomach or small intestine wall is where the majority of gastrointestinal stromal tumours (GISTs) begin to grow. These tumours frequently expand into the GI tract’s free space, so unless they are in a specific area or reach a specific size, they might not immediately cause symptoms.
Small tumours may not show any symptoms and may be unintentionally discovered by the doctor when examining another issue. These little tumours frequently develop slowly.
Small GISTs may cause no symptoms, and they may grow so slowly that they don’t cause problems at first. As a GIST grows, it can cause signs and symptoms. They might include:
- Abdominal pain
- A growth you can feel in your abdomen
- Fatigue
- Nausea
- Vomiting
- Cramping pain in the abdomen after eating
- Not feeling hungry when you would expect to
- Feeling full if you eat only a small amount of food
- Dark-colored stools caused by bleeding in the digestive system
GISTs can happen in people at any age, but they are most common in adults and very rare in children. The cause of most GISTs isn’t known. A small number are caused by genes passed from parents to children.
Symptoms due to blood loss
GISTs tend to be fragile tumors that can bleed easily. In fact, they are often found because they cause bleeding into the GI tract. Signs and symptoms of this bleeding depend on how fast it occurs and where the tumor is located.
- Brisk bleeding into the esophagus or stomach might cause the person to throw up blood. When the blood is thrown up it may be partially digested, so it might look like coffee grounds.
- Brisk bleeding into the stomach or small intestine can make bowel movements (stools) black and tarry.
- Brisk bleeding into the large intestine is likely to turn the stool red with visible blood.
- If the bleeding is slow, it often doesn’t cause the person to throw up blood or have a change in their stool. Over time, though, slow bleeding can lead to a low red blood cell count (anemia), which can make a person feel tired and weak.
Bleeding from the GI tract can be very serious. If you have any of these signs or symptoms, see a doctor right away.
Diagnosis of GIST
GISTs (gastrointestinal stromal tumours) are frequently discovered as a result of signs or symptoms. Other issues are discovered through exams or assessments. However, it’s not always possible to determine with absolute certainty if a person has a GIST or another sort of gastrointestinal (GI) tumour from these symptoms or preliminary tests. If a GI tumour is suspected, more testing will be required to identify it.
Medical history and physical examination
Your medical history, including your symptoms, potential risk factors, family history, and any medical disorders, will be discussed with the doctor.
In order to learn more about any physical symptoms of a GI tumour, such as an abdominal mass, or other health issues, your doctor will perform a physical examination on you.
The doctor will perform imaging tests or endoscopy exams if there is a reason to believe you may have a GIST (or another type of GI tumour) to help determine whether it is cancer or something else. You can be referred to a specialist while seeing your primary care physician, such as a gastroenterologist (a doctor who treats diseases of the digestive system).
If a GIST is discovered, you will probably undergo additional testing to assist identify the cancer’s stage (extent).
Imaging tests
Imaging tests use x-rays, magnetic fields, or radioactive substances to create pictures of the inside of the body. Imaging tests are done for a number of reasons, including:
- To help find out if a suspicious area might be cancer
- To learn how far cancer has spread
- To help determine if treatment has been effective
- To look for signs that the cancer has come back
Most people thought to have a GI tumor will get one or more of these tests.
Computed tomography (CT) scan
A CT scan creates finely detailed cross-sectional images of your body using x-rays. A CT scan produces precise images of the body’s soft tissues, unlike a standard x-ray.
Patients with (or at risk for) GISTs can benefit from CT scans to determine the size and location of a tumour as well as to determine whether it has migrated to other areas of the body.
In some circumstances, CT scans can also be utilised to accurately direct a biopsy needle into a potential cancerous area. These types of biopsies are often performed only if the results can influence the choice of treatment. However, this can be problematic if the tumour may be a GIST (because of the risk of bleeding and a probable increased risk of tumour spread).
Magnetic resonance imaging (MRI) scan
MRI scans produce detailed pictures of the body’s soft tissues, just like CT scans do. However, MRI scans substitute radio waves and powerful magnets for x-rays.
Although CT scans are sufficient most of the time, MRI scans can occasionally be helpful in determining the extent of the cancer in the abdomen in persons with GISTs. MRIs can also be used to check for cancer that has possibly returned (recurred) or spread (metastasized), especially in the brain or spine.
Barium X-Rays
Compared to earlier times, barium x-rays are no longer as frequently employed. They have been mostly supplanted by endoscopy and CT/MRI (where the doctor actually looks inside your esophagus, stomach, and intestines with a narrow fiberoptic scope – see below).
For these kinds of x-rays, the inner lining of the oesophagus, stomach, and intestines are coated with a chalky liquid containing barium. This makes it simpler to see irregular lining sections on an x-ray. These exams are occasionally used to identify GI malignancies, however they sometimes fail to detect small intestine tumours.
Most likely, you will need to begin fasting the evening before the test. You might need to take laxatives and/or enemas to clean out the bowels the night before or the morning of the exam if your colon is being inspected.
Barium swallow
When someone has a swallowing issue, this is frequently the initial test that is performed. You consume a barium-containing beverage to coat the lining of your oesophagus in preparation for this test. The following few minutes are spent taking a series of x-rays.
Upper GI series
With the exception of the fact that x-rays are taken after the barium has had time to cover the stomach and the first portion of the small intestine, this test is comparable to the barium swallow. More x-rays can be taken during the following few hours as the barium travels through to check for issues in the remaining small intestine. An example of this is a little bowel follow-through.
Enteroclysis
Your mouth or nose, oesophagus, stomach, and beginning of the small intestine are all entered through a tiny tube. A substance that increases the amount of air in the intestines and causes them to expand is also delivered through the tube with the barium. The intestines are then radiographed after that. Compared to a small bowel follow-through, this test can provide better views of the small intestine but is also more painful.
Barium enema
This test, sometimes referred to as a lower GI series, examines the large intestine’s inner surface (colon and rectum). While you are reclining on the x-ray table, a short, flexible tube is put in the anus to provide the barium solution for this test. To help move the barium toward the colon wall and better cover the inner surface, air is frequently pumped in through the tube as well. An air-contrast barium enema or double-contrast barium enema is what this is. To help disseminate the barium and to gain multiple perspectives of the colon, you could be requested to adjust your position. After that, x-rays are taken in one or more sets.
Positron emission tomography (PET) scan
You receive an injection containing a mildly radioactive sugar that concentrates mostly in cancer cells in order to have a PET scan. Then, a photograph of the body’s radioactive regions is made using a specific camera. While a PET scan cannot provide the same level of information as a CT or MRI scan, it may simultaneously screen for potential cancer spread throughout the entire body.
Nowadays, many facilities have equipment that can do a PET and CT scan simultaneously (PET/CT scan). This enables the clinician to have a closer look at any regions that “lit up” on the PET scan.
When CT or MRI scan results are unclear, PET scans can be helpful for examining GISTs. This examination can also be done to search for potential sites where the cancer may have metastasized in order to assess whether surgery is an option.
The effectiveness of a pharmacological treatment can also be determined using PET scans, which frequently provide results more quickly than CT or MRI scans. The scan is often performed a few weeks after the medicine is first taken. The tumour will quit absorbing the radioactive sugar if the medication is functioning. Your doctor might decide to alter your medicine therapy if the tumour continues to absorb the sugar.
Endoscopy
A flexible, illuminated tube with a tiny video camera on the end is called an endoscope, and it is inserted into the body during an endoscopy to view the GI tract’s inner lining. Small bits can be biopsied (removed) through the endoscope if abnormal areas are discovered. To determine whether the biopsy samples have cancer and, if so, what form of cancer, it will be examined under a microscope.
GISTs are frequently seen below the mucosa, or outer layer, of the GI tract’s inner lining. As opposed to more frequent GI tract tumours, which often begin in the mucosa, they may be more difficult to see with endoscopy. If a GIST is present, the doctor might only be able to observe a bulge under the generally smooth surface. Additionally, GISTs underneath the mucosa are more difficult to biopsy with an endoscope. This is one of the main causes of undiagnosed GISTs prior to surgery.
There is a higher likelihood that the GIST will spread to other parts of the body if the tumour has penetrated the GI tract’s inner lining and is visible on endoscopy.
Upper endoscopy
In this operation, the inner lining of the oesophagus, stomach, and first segment of the small intestine are examined using an endoscope that is introduced through the mouth and down the neck. Any aberrant sites may be the subject of biopsy samples.
A hospital, an outpatient surgery centre, or a doctor’s office can all do an upper endoscopy. Usually, you receive medication via an intravenous (IV) line to induce sleep prior to the exam. The examination itself typically takes between 10 and 20 minutes, but if a tumour is discovered or biopsy samples need to be collected, the time may increase.
Colonoscopy
A colonoscope, a specific kind of endoscope, is introduced via the anus and up into the colon during a colonoscopy. This enables the physician to examine the colon’s and rectum’s inner lining and collect biopsy samples from any abnormal spots.
It must be thoroughly cleaned before the test in order to gain a clear view of the colon’s interior. You’ll receive detailed instructions from your doctor. Before the test, you might need to adhere to a particular diet for a day or more. Additionally, you might need to consume a significant amount of a liquid laxative the night before, which will need you to spend a lot of time in the restroom.
An outpatient surgery centre, a doctor’s office, or a hospital are all possible places to have a colonoscopy done. Most likely, an intravenous (IV) medication will be administered to you before the treatment to help you feel at ease and asleep. Less frequently, general anaesthesia may be administered to put you into a profound slumber. The examination normally lasts 15 to 30 minutes, but if a tumour is discovered or a sample is required, the time may be extended.
Capsule endoscopy
Both colonoscopy and upper endoscopy are unable to access the entire small intestine. One method of viewing the small intestine is with a capsule endoscope.
An endoscope is not actually used in this process. Instead, a light source and a tiny camera are included in a capsule that you ingest. This capsule is about the size of a large vitamin tablet. The capsule passes through the stomach and into the small intestine like any other pill would. It captures thousands of images while it passes through the intestine, which typically takes around 8 hours. These photos are electronically transferred to a waist-worn device. The doctor can examine the images as a video after downloading them onto a computer. During a typical bowel movement, the capsule leaves the body and is eliminated.
You can carry on with your regular daily activities while the capsule passes through the GI tract since this test doesn’t require sedation. The most effective applications for this relatively new method are still being researched. One drawback is that throughout the test, any aberrant regions that are visible cannot be biopsied.
Double balloon enteroscopy (endoscopy)
This is an alternative perspective on the small intestine. Regular endoscopy cannot provide a thorough examination of the small intestine due to its length and complexity. However, this technique avoids them by utilising a unique endoscope that consists of 2 tubes, one inside the other.
You receive general anaesthetic or intravenous (IV) medication to help you relax (so that you are asleep). Depending on whatever section of the small intestine needs to be inspected, the endoscope is subsequently entered either through the mouth or the anus.
The camera-equipped inner tube is advanced roughly a foot ahead once it is within the small intestine as the doctor examines the lining. The endoscope is then anchored by inflating a balloon on its tip. A second balloon is used to secure the outer tube in place when it is advanced to almost reach the end of the inner tube. The endoscope is again advanced after the first balloon has been inflated. The doctor can visualise the intestine one foot at a time by repeatedly performing this procedure. It can take hours to finish the test.
Along with capsule endoscopy, this test can be performed. The primary benefit of this test over capsule endoscopy is the ability for the physician to do a biopsy if an abnormality is discovered. Because you are given medication to keep you drowsy for the procedure, similar to other forms of endoscopy.
Endoscopic ultrasound (EUS)
This kind of imaging examination makes use of an endoscope. Sound waves are used in ultrasound to take photographs of the body’s organs. A transducer—a wand-like probe—is applied to the skin during the majority of ultrasonic exams. The probe emits sound waves, which are then picked up by a pattern of echoes.
The ultrasonic probe for an EUS is located at the endoscope’s tip. This enables the probe to be positioned very next to (or on top of) a GI tract tumour. The probe emits sound waves and then listens for the echoes that return, much like a conventional ultrasound. The echoes are then converted by a computer into a picture of the area being examined.
The specific position and size of the GIST can be discovered using EUS. It is helpful in determining how far a tumour has encroached on the GI tract wall (or beyond it and into a nearby organ). If the tumour has migrated to neighbouring lymph nodes, the test can also assist identify those nodes. A needle biopsy can also be guided with its assistance (see below). Before this treatment, you will normally get medication to put you to sleep.
Biopsy
Even if an abnormality is seen on an imaging test, such as a CT scan or barium x-ray, these procedures frequently cannot determine with certainty whether the abnormality is a GIST, another sort of tumour (benign or cancerous), or some other ailment (like an infection). Removing cells from the area is the only way to be certain of what it is. This process is known as a biopsy. The cells are then transported to a lab, where a pathologist examines them under a microscope and may do additional tests on them.
Not all patients with tumours that could be GISTs require a biopsy prior to treatment. A biopsy is often only performed if it will aid in determining treatment choices if a doctor suspects a tumour is a GIST. GISTs are frequently weak tumours that are prone to disintegrating and bleeding quickly. Any biopsy must be performed with extreme caution due to the possibility that it could result in bleeding or perhaps raise the danger of cancer spreading.
Endoscopic biopsy
An endoscope can be used to collect biopsy samples. In order to obtain a small sample of the tumour when one is discovered, the doctor can pass biopsy forceps (pincers or tongs) through the tube.
Despite the tiny sample size, doctors may frequently provide a reliable diagnosis. However, with GISTs, the tumour may occasionally be hidden beneath the inner lining of the stomach or intestine, preventing the biopsy forceps from penetrating deep enough to reach it.
Although it is uncommon, bleeding from a GIST following a biopsy can be a major issue. If this happens, medical professionals may use an endoscope to inject medications into the tumour to shrink blood vessels and stop the bleeding.
Needle biopsy
A small sample of the area can also be taken using a thin, hollow needle during a biopsy. When performing an endoscopic ultrasound is the most typical approach to achieve this (described above). A needle on the endoscope’s tip is guided into the tumour by the physician using an ultrasound image as a guide. An endoscopic ultrasound-guided tiny needle aspiration is what this is (EUS-FNA).
Less frequently, the doctor might use an imaging test like a CT scan to guide the placement of a needle through the skin and into the tumour. Percutaneous biopsy is the term used for this.
Surgical biopsy
The doctor can advise waiting until surgery to remove the tumour in order to collect a sample if an endoscopic or needle biopsy is not possible or if the outcome of a biopsy would not impact treatment options.
The procedure is known as a laparotomy if a significant abdominal incision is used to perform the surgery. Occasionally, the tumour can be sampled (or small tumours can be excised) using a laparoscope, a thin, illuminated tube that allows the surgeon to see within the abdomen through a little incision. Using long, thin surgical instruments that are inserted through additional small abdominal incisions, the surgeon can then sample (or remove) the tumour. Laparoscopic or keyhole surgery is the term used for this.
Lab tests
Once tumor samples are obtained, a pathologist might be able to tell that a tumor is most likely a GIST just by looking at the cells with a microscope. But sometimes further lab tests might be needed to be sure.
Immunohistochemistry: For this test, a part of the sample is treated with man-made antibodies that will attach only to a certain protein in the cells. The antibodies cause color changes if the protein is present, which can be seen under a microscope.
If GIST is suspected, some of the proteins most often tested for are KIT (also known as CD117) and DOG1. Most GIST cells have these proteins, but cells of most other types of cancer do not, so tests for these proteins can help tell whether a GI tumor is a GIST or not. Other proteins, such as CD34, might be tested for as well.
Molecular genetic testing: Testing might also be done to look for mutations in the KIT or PDGFRA genes, as most GIST cells have mutations in one or the other. Testing for mutations in these genes can also help determine if certain targeted therapy drugs are likely to be helpful in treating the cancer.
Less often, tests might be done to look for changes in other genes, such as the SDH genes.
Mitotic rate: If a GIST is diagnosed, the doctor will also look at the cancer cells in the sample to see how many of them are actively dividing into new cells. This is known as the mitotic rate (or mitotic index). A low mitotic rate means the cancer cells are growing and dividing slowly, while a high rate means they are growing quickly. The mitotic rate is an important part of determining the stage of the cancer.
Blood tests
Your doctor may order some blood tests if they think you may have a GIST.
There are no blood tests that can tell for sure if a person has a GIST. But blood tests can sometimes point to a possible tumor (or to its spread). For example:
- A complete blood count (CBC) can show if you have a low red blood cell count (that is, if you are anemic). Some people with GISTs may become anemic because of bleeding from the tumor.
- Abnormal liver function tests may mean that the GIST has spread to your liver.
Blood tests are also done to check your overall health before surgery or while you get other treatments, such as targeted therapy.
Treatment of GIST’s
Surgery for GIST’s
When a tumour is small, it is frequently possible to remove it together with a small patch of healthy tissue surrounding it. This is accomplished by making an incision in the skin. Since GISTs nearly never migrate to the lymph nodes, unlike many other malignancies, there is typically no need to remove the lymph nodes in the area.
“Keyhole” (laparoscopic) surgery is an option for some tiny malignancies. To remove the tumour, multiple small incisions are performed rather than one large one. A laparoscope, a narrow, illuminated tube with a tiny video camera on the end, is inserted by the surgeon via one of them. This enables them to view the abdomen. The tumour is then removed using long, thin surgical instruments through the other wounds. Patients typically recover more quickly from this sort of surgery than from conventional surgery, which requires a larger incision, because the incisions are smaller.
Surgery for larger GIST’s
The surgeon could still be able to completely remove the tumour even if it is huge or spreading to other organs. It could be necessary to remove a portion of the intestines or other organ to do this. Additionally, the surgeon may remove malignancies that have migrated to the liver or other organs in the abdomen.
Taking the targeted medication imatinib (Gleevec) initially, often for at least a few months, may be another option for cancers that are big or have spread into neighbouring areas. Neoadjuvant therapy, as it is known, frequently causes the tumour to shrink, making surgery to remove it easier.
Surgery for metastatic GISTs
For a GIST that has expanded (metastasized) to other areas of the body, surgery is not a usual treatment. The initial line of treatment for metastatic GISTs is typically targeted therapy medications. However, some medical professionals could suggest surgery to remove the metastatic tumours if there are only a few of them and they react well to targeted therapy. Although no sizable research have been conducted to demonstrate how useful this is, it may be a choice. If your doctor recommends this procedure, be sure you are aware of its objectives and any potential negative effects.
Other alternatives could include various local treatments like embolization or ablation if the liver-based malignancies are difficult to remove.
Ablation and embolization to treat gastrointestinal stromal tumors
Treatments like ablation and embolization may be utilised if a gastrointestinal stromal tumour (GIST) has progressed to the liver, especially if surgery is unable to eliminate the tumours.
Ablation
Ablation is the term for the removal of tumours through the use of chemicals, high temperatures, or both. It can occasionally be utilised to eliminate GISTs that have only developed a few little tumours in the liver. Ablation might not be the best option for treating tumours close to critical structures like major blood arteries, the diaphragm (the thin breathing muscle above the liver), or major ducts in the liver because it frequently destroys some of the normal tissue surrounding the tumour.
There are several types of ablation:
- Radiofrequency ablation (RFA), which uses high-energy radio waves to heat the tumor and destroy cancer cells
- Ethanol (alcohol) ablation, where concentrated alcohol is injected directly into the tumor to kill cancer cells
- Microwave thermotherapy, where microwaves transmitted through a probe placed in the tumor are used to heat and destroy the cancer cells
- Cryosurgery (cryotherapy), which destroys a tumor by freezing it using a thin metal probe,. This method sometimes requires general anesthesia (you are in deep sleep and not able to feel pain)
Embolization
Embolization is a treatment in which the doctor administers medications in an effort to stop or lessen the blood flow to cancerous liver cells.
Given that it contains two blood supply, the liver is uncommon. Branches of the portal vein feed the majority of normal liver cells, whereas branches of the hepatic artery often feed the majority of cancerous liver cells. The majority of healthy liver cells are not damaged because they receive their blood supply through the portal vein; however, blocking the branch of the hepatic artery feeding the tumour does aid in the death of the cancer cells.
Embolization does restrict part of the blood flow to the healthy liver tissue, thus it may not be a good option for some individuals whose livers have already suffered liver damage from conditions like cirrhosis or hepatitis.
Targeted therapy for GIST’s
Certain proteins that aid in cell division and growth in gastrointestinal stromal tumour (GIST) cells can be targeted by some medications. When treating GISTs, these focused medications—also known as precision medications—are frequently highly beneficial. They function differently than conventional chemotherapy (chemo) medications, which are typically ineffective.
Tyrosine kinase inhibitors (TKIs) are the name given to the targeted medications used to treat GISTs because they specifically target proteins known as KIT and PDGFRA, which are tyrosine kinases.
These targeted medications are all given orally, often once per day.
Targeted therapy drugs used for treatment of GIST’s:
- Imatinib
- Sunitinib
- Regorafenib
- Ripretinib
- Avapritinib
- Sorafenib (Nexavar)
- Nilotinib (Tasigna)
- Dasatinib (Sprycel)
- Pazopanib (Votrient)
Chemotherapy
Drugs are used in chemotherapy, also known as “chemo,” to treat cancer. These medications are frequently administered intravenously (IV) or orally. This medication may be helpful for malignancies that have spread past the organ they originated in because they enter the bloodstream and circulate throughout the body.
Chemotherapy refers to the use of any drug to treat cancer, including targeted therapy medications like imatinib (Gleevec), which are now frequently used to treat gastrointestinal stromal tumours (GISTs). However, the term “chemo” is typically used to refer to specific medications that target rapidly proliferating cells anywhere in the body, including cancer cells.
Radiation therapy for GIST’s treatment
High-energy x-rays (or other particles) are used in radiation treatment to kill cancer cells. Radiation is not frequently utilised since it is not particularly effective in treating gastrointestinal stromal tumours (GISTs). However, it can occasionally be used to treat symptoms like bone discomfort.
The radiation experts will take precise measurements before the start of your treatment to determine the right angles for aiming the radiation beams and the right amount of radiation. Imaging tests like CT or MRI scans are frequently performed as part of this planning session, known as simulation.
Similar to receiving an x-ray, radiation therapy uses greater radiation. The actual procedure is painless. Even though the setup process—getting you situated for treatment—usually takes longer, it only takes a few minutes. Radiation therapy may go for several days straight.
- Comments Closed
- June 30th, 2022



Latest Posts
- LungVax: Lung cancer vaccine
- Successful CRISPR Gene Therapies in Practice: Case Studies
- Gamma Delta (γδ) T cells as a potential treatment for glioblastoma
- World-first lung cancer vaccine trials started in seven countries
- Lazertinib with amivantamab-vmjw is approved by the USFDA for non-small lung cancer
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (58)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (790)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (104)
- Cervical cancer (41)
- Chemotherapy (37)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (20)
- Endometrial cancer (10)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (2)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (48)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (45)
- Liver cancer (94)
- Lung cancer (69)
- Lymphoma (46)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (23)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (12)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (8)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (747)
- Treatment in China (647)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview