Beta thalassemia
What is beta thalassemia major?
What is beta thalassemia in children?
Beta thalassemia is a blood condition that is genetic. That implies it is passed down via the genes of the parent. It’s a form of anemia. Anemia is a reduced level of red blood cells or low hemoglobin. A part of red blood cells is hemoglobin. It carries muscles, tissues and cells with oxygen. Beta thalassemia affects hemoglobin development.
Different forms of thalassemia occur. The magnitude of your child’s anemia depends on the type you have.
What causes beta thalassemia in a child?
Beta thalassemia is caused by a gene defect which controls the production of hemoglobin. Three forms exist:
- Beta thalassemia major (Cooley’s anemia) : This is the type of beta thalassemia that is most extreme. During the first 2 years of life, it is sometimes noticed. Kids also need regular transfusions of blood. This can cause severe iron overload issues that are normal.
- Beta thalassemia intermedia : This type of thalassemia is widespread all over the world. Abnormal hemoglobin may also cause it. Or there may be more than one kind of abnormal hemoglobin present. It is often detected later than major beta thalassemia. Typically, transfusions are not required.
- Thalassemia minor or thalassemia trait : These are the carriers of beta thalassemia.
Which children are at risk for beta thalassemia?
Beta thalassemia is a condition that is genetic. It is transmitted from parents to kids.
- When two carrier parents who have thalassemia minor pass it on to their infant, thalassemia major is inherited. Each of the two carrier parents’ children has a 25% beta thalassemia major.
- When two carrier parents transmit it to their infant, Thalassemia minor is inherited. There is a 50 percent risk of getting beta thalassemia minor in each child of two carrier parents.
In the following individuals, the gene defect that causes beta thalassemia is more common:
- Greek
- Italian
- Middle Eastern
- Asian
- African
What are the symptoms of beta thalassemia in a child?
The symptoms of beta thalassemia major occur when an infant is between 6 and 24 months. They include:
- Poor growth and development
- Pale skin
- Feeding problems
- Diarrhea
- Irritability, fussiness
- Fevers
- Enlarged abdomen from enlarged spleen
The symptoms of beta thalassemia intermedia happen at a later age and include:
- Pale or yellow skin
- Gallstones
- Enlarged liver and spleen
- Bone changes
- Leg ulcers or sores
- Soft bones
Children with beta thalassemia minor have anemia, but often do not have symptoms.
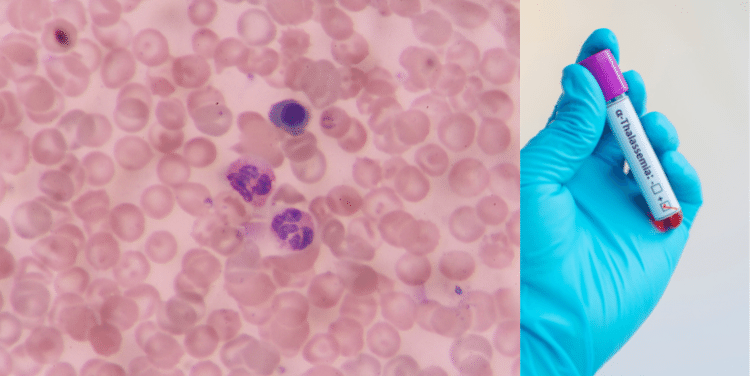
Diagnosis of beta thalassemia in a child
The healthcare professional will be asking about the signs and health history of your infant. He or she is going to give your child a physical test. Your child will have assessments as well such as:
- Complete blood count (CBC) :The red and white blood cells, blood clotting cells (platelets) and occasionally, young red blood cells are tested by a full blood count. Hemoglobin and hematocrit are included and the red blood cells are more detailed.
- Peripheral smear :To see if they appear odd, a tiny amount of blood is examined under a microscope.
- Hemoglobin electrophoresis. This test measures the types and amount of hemoglobin.
- Iron studies. These studies check for iron deficiency anemia.
- DNA testing. These tests look for gene defects. DNA testing can find alpha thalassemia carriers.
Beta thalassemia major treatment in a child
Treatment will depend upon the symptoms, age, and general health of your child. It will also rely on how serious the disease is.
The healthcare provider for your child would possibly refer you to a hematologist. He’s a blood disorder specialist. Beta thalassemia treatment depends on the type. It can involve:
- For beta thalassemia major:
- Regular blood transfusions (your child gets healthy blood from a donor)
- Your child needs to have completed the hepatitis B vaccine series.
- Medicines (to cut amount of iron in the body, called chelation therapy)
- Stem cell or cord blood transplant
- Other therapies are under study, including gene therapy.
- For beta thalassemia intermedia:
- Possible blood transfusions
- Removal of the spleen
- Daily doses of folic acid, a vitamin needed to make hemoglobin
Complications of beta thalassemia in a child
Complications from frequent transfusions may happen when a child is about 10 or 11 years old. They are from having too much iron. The complications include:
- Delayed growth and development, including sexual development
- Heart, liver, and spleen problems
- Endocrine system problems (for example, diabetes or thyroid problems)
- Blood clots
- Osteoporosis
Children with beta thalassemia intermedia may also have complications from iron overload.
How can I help my child live with beta thalassemia?
The ongoing care of your child should include:
- Regular physical exams
- Regular blood work
- Avoiding iron supplements
Talk with your provider about genetic counseling.
When should I call my child’s healthcare provider?
Each child’s symptoms and treatment is different. Make sure you understand your child’s symptoms and treatment, including possible side effects. Call your child’s provider if you notice any changes or have questions. For example, call the provider if your child has any of the following:
- Slowed growth or development
- Feeding problems
- Fussiness
- Fevers
Key points about beta thalassemia in children
- Beta thalassemia is an inherited blood disorder in which a child has anemia.
- It is caused by genetic defects that control the production of hemoglobin.
- The types are beta thalassemia major, intermedia, and minor.
- Treatment includes regular blood transfusions.
- Treatment for iron overload is needed after years of transfusions.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
What Are the Different Types of Beta Thalassemia?
The three types of beta thalassemia are:
- Beta thalassemia minor (also called beta thalassemia trait) : People with minor beta thalassemia may have mild anemia, but no medical care is generally required.
- Beta thalassemia intermedia :People with intermediate beta thalassemia have moderately serious anemia, and daily blood transfusions and other medical care may be required for some. Blood transfusions provide the body with good hemoglobin and RBCs.
- Beta thalassemia major(also called Cooley’s anemia): Significant symptoms and life-threatening anemia are present in people with major beta thalassemia. Regular blood transfusions and other medical services are required for them.
Signs & symptoms of beta thalassemia
There are typically no signs in people with the beta thalassemia trait.
Children with moderate or major beta thalassemia may have no symptoms at birth, but they typically develop in the first 2 years of life. They may have anemia signs, such as:
- tiredness
- shortness of breath
- a fast heartbeat
- pale skin
- yellow skin and eyes (jaundice)
- moodiness
- slow growth
People with large or moderate beta thalassemia normally have an excess of iron in the body, either from the disorder itself or from frequent blood transfusions. The heart, liver, and endocrine system can be impaired by excess iron.
People with significant beta thalassemia can have some serious problems with their health, including:
- bone deformities and broken bones from changes in the bone marrow (where RBCs are made)
- an enlarged spleen because the organ works harder than normal. Doctors might need to remove the spleen if it gets too big.
- infections, especially if doctors removed the spleen (the spleen helps fight some infections)
Causes of beta thalassemia
Two alpha proteins and two beta proteins are made from hemoglobin. A gene alteration (mutation) causes alpha thalassemia in the alpha proteins. Beta thalassemia induces a gene alteration in the beta proteins.
The gene alteration induces an excess of hemoglobin proteins in beta thalassemia. The imbalance induces anemia because:
- Red blood cells break down faster than normal.
- Fewer RBCs are made.
- Less hemoglobin is made.
The imbalance also leads to medical problems in the bones, bone marrow, and other organs.
Who Gets Beta Thalassemia?
People inherit from their parents the genes for beta thalassemia. A kid gets one of the mother’s beta protein genes and one of the father’s:
- Someone who inherits the gene change in the beta protein from one parent has beta thalassemia minor (beta thalassemia trait).
- Someone who inherits a gene change in both beta proteins (one from each parent) has beta thalassemia intermedia or beta thalassemia major (Cooley’s anemia).
Often with a sickle cell gene change, a beta thalassemia gene change may be inherited. Sickle beta thalassemia, a form of disease of sickle cells, results in this. A genetic counselor will help families to understand how beta thalassemia functions in families in various ways.
How Is Beta Thalassemia Diagnosed?
Doctors will examine the fetus if a woman is pregnant and both parents have a beta thalassemia trait:
- Chorionic villus sampling (CVS): This includes taking a small portion of the placenta for examination, performed about 11 weeks into pregnancy.
- Amniocentesis: This includes removing a sample of the fluid that covers the fetus to search for signs of complications, usually performed around 16 weeks into the pregnancy.
Young children may be diagnosed with a blood test if they have anemia, a bloated stomach (when the spleen is enlarged), or poor development. Either or more of these are used in the blood tests:
- hemoglobin electrophoresis
- test for abnormal hemoglobin genes
How Is Beta Thalassemia Treated?
Treatment relies on the type of beta thalassemia that someone has.
Children with beta thalassemia typically do not require counseling.
Children and adults majoring in beta thalassemia require lifelong medical treatment, including:
- regular blood transfusions about every 2-4 weeks
- medicines to remove extra iron from their bodies (called chelation)
Individuals with intermediate beta thalassemia may require blood transfusions and chelation, but not as much as those with major beta thalassemia.
Beta thalassemia is not healed by blood transfusions and chelation. It can be treated by a stem cell transplant, but it is a severe operation with many complications and will not help anyone with the disease. In order to support people with beta thalassemia, physicians and scientists are focusing on developing gene therapy and other treatments.
How Can Parents Help Kids With Beta Thalassemia Trait?
There’s no special treatment needed for a child who has a beta thalassemia trait. To understand how beta thalassemia functions in families, your child will want to talk to a genetic counselor someday.
Be sure to tell all health care professionals that there is a beta thalassemia trait in your infant. This way, the professionals will know the cause when mild anemia occurs during blood tests.
How Can Parents Help Kids With Beta Thalassemia Intermedia or Major?
Children with intermediate or major beta thalassemia need lifelong medical treatment. With routine health care, children with intermediate and major beta thalassemia will live well into their 50s. Normal medical treatment, which involves transfusions and chelation, is the safest way for your child to live his or her healthiest life.
Establishing a health care team for your child is critical. The center will help you bring the team together if you live near a Thalassemia Treatment Center. The team ought to include:
- a hematologist (a doctor who specializes in blood disorders)
- doctors to treat problems from iron overload, including:
- an endocrinologist(a doctor who specializes in organs that make hormones)
- a cardiologist(heart doctor)
- a gastrointestinal doctor (a doctor who specializes in the digestive tract)
- an infectious disease doctor to help treat any infections
- a dietitian to help with meal planning and any vitamin supplements that are needed
- a primary care doctor to help with routine care
- a case manager (a nurse or other provider who coordinates your child’s medical care)
- a social worker to help with insurance information and your child’s schooling, and to support you, your child, and your family
- a psychologist to help caregivers and your child cope with thalassemia
What Else Should I Know?
When your child has moderate beta thalassemia or major beta thalassemia, handling medical treatment and the emotions and feelings that come with the disease can be a struggle for your family. It can lead to:
- Find support through:
- your child’s care team, especially the social worker or psychologist
- other families who have a child with beta thalassemia
- friends and family
- Help your child see the opportunities he or she has, not the limitations.
- Manage your own stress level by taking care of yourself and doing things that you enjoy.
- Include siblings of the child with thalassemia. Show them that they can have a role, such as keeping their sibling company during transfusions or just being there to listen.
- Comments Closed
- September 2nd, 2020


Latest Posts
- Targeting FGFR4 and CD276 with CAR T-cells demonstrates a strong antitumor impact against children rhabdomyosarcoma
- Disruption of CD5 on CAR T Cells Enhances the Effectiveness of Anti-Tumor Treatment
- The future of gene therapy: What to expect in the next decade?
- Unlocking the genetic code: The future of gene therapy for genetic disorders
- CRISPR and gene editing: Revolutionizing gene therapy
- Aids cancer (4)
- Anal cancer (8)
- Anemia (5)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Bladder cancer (10)
- Blog (3)
- Blood cancer (56)
- Bone cancer (11)
- Bone marrow transplant (43)
- Brain Tumor (48)
- Breast Cancer (48)
- Cancer (787)
- Cancer surgery (234)
- Cancer treatment in South Korea (341)
- cancer treatment in Thailand (331)
- Cancer treatment in Turkey (329)
- Cancer treatment in USA (328)
- CAR NK-Cell therapy (12)
- CAR T-Cell therapy (95)
- Cervical cancer (41)
- Chemotherapy (36)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (5)
- Colon cancer (95)
- Coronavirus (1)
- Cosmetic surgery (7)
- COVID19 (2)
- Doctor (37)
- Drugs (19)
- Endometrial cancer (9)
- Esophageal cancer (15)
- Eye cancer (9)
- Gall bladder cancer (3)
- Gastric cancer (22)
- Glioblastoma (1)
- Gynecological cancer (2)
- Head and neck cancer (20)
- Hematological Disorders (50)
- Hospital (47)
- Immunotherapy (25)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (44)
- Liver cancer (94)
- Lung cancer (65)
- Lymphoma (44)
- MDS (2)
- Medical tourism (71)
- Medical visa (11)
- Melanoma (8)
- Merkel cell carcinoma (1)
- Mesothelioma (4)
- Myeloma (22)
- Oral cancer (13)
- Ovarian Cancer (13)
- Pancreatic cancer (39)
- Penile cancer (1)
- Procedure (19)
- Prostrate cancer (10)
- Proton therapy (26)
- Radiotherapy (35)
- Rectal cancer (57)
- Sarcoma (11)
- Skin Cancer (13)
- Spine surgery (8)
- Stomach cancer (40)
- Surgery (54)
- Systemic mastocytosis (1)
- T Cell immunotherapy (2)
- T-Cell therapy (7)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (14)
- Treatment (746)
- Treatment in China (646)
- Treatment in India (684)
- Treatment in Israel (586)
- Treatment in Malaysia (360)
- Treatment in Singapore (255)
- Treatment in South Korea (238)
- Treatment in Thailand (233)
- Treatment in Turkey (233)
- Uncategorized (39)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (3)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)






Privacy Overview