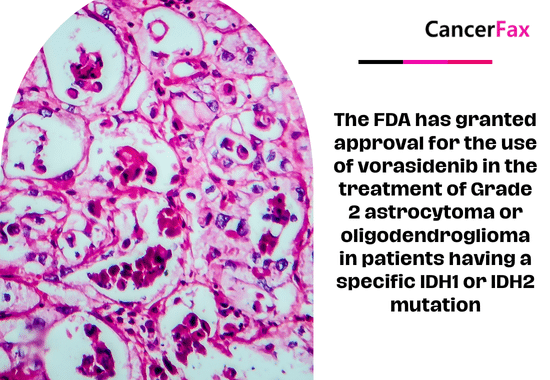
August 2024: Vorasidenib (Voranigo, Servier Pharmaceuticals LLC), an inhibitor of isocitrate dehydrogenase-1 (IDH1) and isocitrate dehydrogenase-2 (IDH2), has been approved by the Food and Drug Administration for the treatment of Grade 2 astrocytoma or oligodendroglioma in adult and pediatric patients aged 12 and older. This approval is specifically for patients with a susceptible IDH1 or IDH2 mutation who have undergone surgery, including biopsy, sub-total resection, or gross total resection.
This marks the initial endorsement by the FDA of a systemic treatment for patients diagnosed with Grade 2 astrocytoma or oligodendroglioma, who possess a vulnerable IDH1 or IDH2 mutation.
Safety and Efficacy
The effectiveness of the treatment was assessed in 331 individuals who had Grade 2 astrocytoma or oligodendroglioma and had a susceptible IDH1 or IDH2 mutation. These patients participated in a clinical trial called INDIGO (NCT04164901), which was a randomized, multicenter, double-blind, placebo-controlled study. The patients were randomly assigned in a 1:1 ratio to receive either vorasidenib 40 mg orally once daily or a placebo orally once daily until there was disease progression or intolerable toxicity.
The mutation status of IDH1 or IDH2 was determined in advance using the Oncomine Dx Target Test by Life Technologies Corporation. Patients who were assigned to receive a placebo were given the option to switch to vorasidenib treatment after their illness progression was confirmed through radiographic imaging. Patients who had already undergone anti-cancer treatment, such as chemotherapy or radiation therapy, were not included.
The primary measure of effectiveness was progression-free survival (PFS) assessed by a blinded independent review committee according to the modified Response Assessment in Neuro-Oncology for Low Grade Glioma (RANO-LGG) criteria. Another measure of effectiveness was the duration until the next intervention. The hazard ratio for progression-free survival (PFS) was 0.39 with a 95% confidence interval (CI) of 0.27 to 0.56. The p-value was less than 0.0001. The vorasidenib arm did not achieve the median time to next intervention, while the placebo arm had a median duration of 17.8 months (HR=0.26; 95% CI: [0.15, 0.43], p <0.0001).
The predominant (≥15%) negative responses seen were fatigue, headache, COVID-19 infection, musculoskeletal pain, diarrhea, nausea, and seizures. The prevailing Grade 3 or 4 laboratory abnormalities, occurring in more than 2% of cases, included elevated alanine aminotransferase, elevated aspartate aminotransferase, increased GGT, and a reduced neutrophil count.
The suggested vorasidenib dosage for adult patients is 40 mg taken orally once a day until there is disease progression or the presence of intolerable toxicity. The appropriate dosage of vorasidenib for pediatric patients aged 12 years and older is determined by their body weight.
For patients who weigh 40 kilograms or more, the recommended dosage is 40 milligrams taken orally once a day.
For patients who weigh less than 40 kg, the recommended dosage is 20 mg taken orally once daily.



Brain cancer precision medicine, Grade 2 astrocytoma drugs, IDH1 mutant glioma treatment, IDH2 inhibitor therapy, Low-grade glioma breakthrough, Oligodendroglioma targeted therapy, Vorasidenib clinical benefits, Vorasidenib FDA approval
CancerFax is the most trusted online platform dedicated to connecting individuals facing advanced-stage cancer with groundbreaking cell therapies.
Send your medical reports and get a free analysis.
🌟 Join us in the fight against cancer! 🌟
Привет,
CancerFax — это самая надежная онлайн-платформа, призванная предоставить людям, столкнувшимся с раком на поздних стадиях, доступ к революционным клеточным методам лечения.
Отправьте свои медицинские заключения и получите бесплатный анализ.
🌟 Присоединяйтесь к нам в борьбе с раком! 🌟