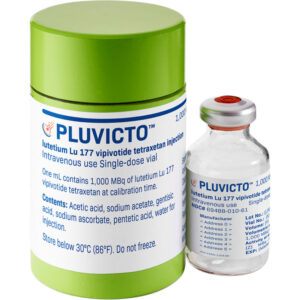
Pluvicto is approved by FDA for metastatic castration-resistant prostate cancer
April 2022: The Food and Drug Administration approved Pluvicto (lutetium Lu 177 vipivotide tetraxetan, Advanced Accelerator Applications USA, Inc., a Novartis company) for the treatment of adult patients with prostate-specific membrane antigen (PSMA)-positive metastatic castration-resistant prostate cancer (mCRPC) who have been treated with androgen receptor (AR) pathway inhibition and taxane-based chemotherapy.
On the same day, the FDA approved Locametz (gallium Ga 68 gozetotide), a radioactive diagnostic agent for positron emission tomography (PET) of PSMA-positive lesions, including selection of patients with metastatic prostate cancer for whom lutetium Lu 177 vipivotide tetraxetan PSMA-directed therapy is indicated. Locametz is the first radioactive diagnostic agent approved for patient selection in the use of a radioligand therapeutic agent.
Patients with previously treated mCRPC should be selected for treatment with Pluvicto using Locametz or another approved PSMA-11 imaging agent based on PSMA expression in tumors. PSMA-positive mCRPC was defined as having at least one tumor lesion with gallium Ga 68 gozetotide uptake greater than normal liver. Patients were excluded from enrollment if any lesions exceeding certain size criteria in the short axis had uptake less than or equal to uptake in normal liver.
Efficacy was evaluated in VISION (NCT03511664), a randomized (2:1), multicenter, open-label trial that evaluated Pluvicto plus best standard of care (BSoC) (n=551) or BSoC alone (n=280) in men with progressive, PSMA-positive mCRPC. All patients received a GnRH analog or had prior bilateral orchiectomy. Patients were required to have received at least one AR pathway inhibitor, and 1 or 2 prior taxane-based chemotherapy regimens. Patients received Pluvicto 7.4 GBq (200 mCi) every 6 weeks for up to a total of 6 doses plus BSoC or BSoC alone.
The trial demonstrated a statistically significant improvement in the primary endpoints of overall survival (OS) and radiographic progression-free survival (rPFS). Hazard ratio (HR) for OS was 0.62 (95% CI: 0.52, 0.74; p<0.001) for the comparison of Pluvicto plus BSoC versus BSoC. Median OS was 15.3 months (95% CI: 14.2, 16.9) in the Pluvicto plus BSoC arm and 11.3 months (95% CI: 9.8, 13.5) in the BSoC arm, respectively. Interpretation of the magnitude of the rPFS effect was limited due to a high degree of censoring from early drop out in the control arm.
The most common adverse reactions (≥20%) occurring at a higher incidence in patients receiving Pluvicto were fatigue, dry mouth, nausea, anemia, decreased appetite, and constipation. The most common laboratory abnormalities that worsened from baseline in ≥30% of patients receiving Pluvicto were decreased lymphocytes, decreased hemoglobin, decreased leukocytes, decreased platelets, decreased calcium, and decreased sodium. Treatment with Pluvicto may result in risk from radiation exposure, myelosuppression, and renal toxicity. The safety follow-up duration in VISION was not sufficient to capture late radiation-associated toxicities.
The recommended Pluvicto dose is 7.4 GBq (200 mCi) intravenously every 6 weeks for up to 6 doses, or until disease progression or unacceptable toxicity.
View full prescribing information for Pluvicto. View full prescribing information for Locametz.
Dr. Nishant Mittal is a highly accomplished researcher with over 13 years of experience in the fields of cardiovascular biology and cancer research. His career is marked by significant contributions to stem cell biology, developmental biology, and innovative research techniques.
Research Highlights
Dr. Mittal's research has focused on several key areas:
1) Cardiovascular Development and Regeneration: He studied coronary vessel development and regeneration using zebrafish models1.
2) Cancer Biology: At Dartmouth College, he developed zebrafish models for studying tumor heterogeneity and clonal evolution in pancreatic cancer.
3) Developmental Biology: His doctoral work at Keio University involved identifying and characterizing medaka fish mutants with cardiovascular defects.
4) Stem Cell Research: He investigated the effects of folic acid on mouse embryonic stem cells and worked on cryopreservation techniques for hematopoietic stem cells.
Publications and Presentations
Dr. Mittal has authored several peer-reviewed publications in reputable journals such as Scientific Reports, Cardiovascular Research, and Disease Models & Mechanisms1. He has also presented his research at numerous international conferences, including the Stanford-Weill Cornell Cardiovascular Research Symposium and the Weinstein Cardiovascular Development Conference.
In summary, Dr. Nishant Mittal is a dedicated and accomplished researcher with a strong track record in cardiovascular and cancer biology, demonstrating expertise in various model systems and a commitment to advancing scientific knowledge through innovative research approaches.
- Comments Closed
- May 5th, 2022



gallium Ga 68 gozetotide, Locametz, lutetium Lu 177 vipivotide tetraxetan, mCRPC, Novartis, Pluvicto, PSMA
CancerFax is the most trusted online platform dedicated to connecting individuals facing advanced-stage cancer with groundbreaking cell therapies.
Send your medical reports and get a free analysis.
🌟 Join us in the fight against cancer! 🌟
Привет,
CancerFax — это самая надежная онлайн-платформа, призванная предоставить людям, столкнувшимся с раком на поздних стадиях, доступ к революционным клеточным методам лечения.
Отправьте свои медицинские заключения и получите бесплатный анализ.
🌟 Присоединяйтесь к нам в борьбе с раком! 🌟