
Review and Prospect of Brain Glioma Treatment in China
Brain Glioma
Brain glioma is one of the most common malignant tumors of the central nervous system. Despite numerous challenges in the treatment field, scientific advancements recently have brought new hope to patients. This article reviews the latest research achievements and clinical progress in brain glioma treatment in 2024.
- Core Advances in Brain Glioma Treatment in 2024
- Surgical Treatment: Precise Resection Combined with Molecular Pathology
Technological Breakthroughs in brain glioma patient
High-resolution imaging techniques: Functional MRI and intraoperative navigation have improved the precision of tumor boundary localization, maximizing protection of neurological functions (e.g., language and motor areas).
Awake surgery combined with intraoperative MRI enables real-time evaluation of resection margins during surgery, reducing the risk of postoperative neurological deficits.
Research Breakthroughs in the treatment Glioma
The RANO Resection Group Study, published in Lancet Oncology, established the first molecular pathology-based surgical evaluation system, confirming a significant positive correlation between tumor resection extent and patient survival (e.g., more pronounced benefits in IDH-mutant patients).
Radiation Therapy: Precision and Protection for Young Patients
Stereotactic Radiotherapy (SRS): High-precision radiation targets tumors specifically, suitable for small-volume gliomas and minimizing damage to normal tissues.
Proton Therapy: Utilizes the “Bragg peak” of proton beams to kill tumor cells precisely, particularly reducing radiation damage to brain tissue in children and young patients. Clinical data show proton therapy prolongs survival and reduces side effects.
Chemotherapy: Optimization of Traditional Drugs and Novel Delivery Systems
Temozolomide (TMZ): Remains the standard chemotherapy for high-grade gliomas, with stable efficacy when combined with radiotherapy.
Nanomedicine Delivery Systems: Targeted drug delivery to tumor sites enhances local drug concentration while reducing systemic toxicity. Preliminary studies indicate that this technology has the ability to penetrate the blood-brain barrier, providing new hope for patients who are resistant to conventional treatments.
Targeted Therapy: The Inauguration of Precision Medicine
Vorasidenib: In the INDIGO study for patients with IDH-mutant low-grade gliomas, the time without disease progression was extended to 27.7 months, which is much better than what traditional therapies offer.
Bernitinib: Approved in April 2024 for adult patients with IDH-mutant astrocytoma (WHO grade 4) or glioblastoma that has a history of low-grade tumors and has PTPRZ1-MET fusion genes, it addresses the need for targeted therapy in the MET pathway.
Ripretinib is included in the NCCN guidelines, demonstrating an objective response rate (ORR) of 58% in NTRK fusion-positive solid tumors and expanding pan-cancer treatment applications.
Niraparib: 2024 ASCO data showed promising results in newly diagnosed MGMT-nonmethylated GBM, with a median overall survival (OS) of 20.3 months, challenging traditional treatment logic based on methylation status.
Immunotherapy: Multi-Target Exploration and Microenvironment Regulation
CAR-T Cell Therapy
EGFRvIII target: A study in the New England Journal of Medicine showed significant short-term efficacy, with rapid tumor burden reduction in some patients.
IL-13Rα2-CAR-T: Nature Medicine data showed a median OS of 7.7 months, breaking through immunotherapy challenges in GBM.
Oncolytic Virus Therapy
HHSV1-TK and Flt3L adenovirus: A study in Lancet Oncology found that patients lived an average of 21.3 months longer, improving treatment by boosting the immune system.
CAN-3110 virus: A Nature report demonstrated safety and efficacy in recurrent GBM, inducing tumor immunogenic cell death.
Tumor Treating Fields (TTFields): Elevated Guideline Status
Both the NCCN Guidelines 2024 V3 and the Chinese CACA Brain Glioma Treatment Guidelines recommend using TTFields as a top treatment option for newly diagnosed GBM, highlighting its benefits in improving survival (like an overall survival of more than 20 months when used with TMZ) and its non-invasive approach.
Future Prospects: Research Directions and Challenges for 2025
Refined Molecular Subtyping: Integrating multi-omics (genomics, proteomics, metabolomics) to further subclassify gliomas and achieve “one-patient-one-treatment” precision therapy.
Combination Therapies: Exploring synergies between targeted therapy, immunotherapy, and TTFields (e.g., Vorasidenib combined with PD-1 inhibitors to reverse immune microenvironment suppression).
Drug Resistance Mechanisms: Unraveling resistance pathways (e.g., PI3K/AKT/mTOR) in refractory subtypes (e.g., IDH wild-type, MGMT nonmethylated) and developing novel inhibitors.
Novel Delivery Technologies: Optimizing blood-brain barrier penetration of nanomedicines and viral vectors while reducing systemic toxicity.
Artificial Intelligence (AI) Applications: AI-assisted imaging diagnosis (e.g., preoperative tumor boundary prediction) and personalized treatment planning (e.g., radiation dose optimization) to enhance clinical decision-making efficiency.
Pediatric Glioma Research: Developing low-toxic, high-efficacy therapies for young patients to minimize radiation impact on brain development (e.g., widespread proton therapy, drugs targeting H3K27M mutation). In 2024, the way we treat brain gliomas shifted from trying to remove as much of the tumor as possible to using a more precise method that combines surgery, radiation, medication, and new technologies like TTFields and CAR-T. Even though there are still challenges (like the blood-brain barrier and immune escape), the approval of targeted drugs (like Bernitinib), new advancements in immunotherapy, and the inclusion of TTFields in guidelines indicate that the field is making rapid progress.
Even though there are still difficulties (like the blood-brain barrier and immune escape), the approval of targeted drugs (like Bernitinib), new developments in immunotherapy, and the acceptance of TTFields in guidelines show that the field is progressing quickly.
By 2025, interdisciplinary collaboration and technological innovation are expected to bring more personalized, efficient, and low-toxic treatment options, gradually moving toward the goal of “chronic disease management” for glioma patients.
Here are the top neurosurgery hospitals in Shanghai and Beijing:
Shanghai
Huashan Hospital Affiliated to Fudan University

Department Strength: Established in 1952, it is a key clinical discipline under the Ministry of Health and a “National Clinical Key Specialty.” Ranked 2nd nationwide in the 2022 neurosurgery specialty comprehensive ranking. It has created multiple firsts in the history of neurosurgery in China, performing over 100,000 neurosurgical operations, and has always been at the advanced level domestically and internationally in clinical care, scientific research, and teaching.
Specialties: Covers all fields of minimally invasive neurosurgery, molecular neurosurgery, functional neurosurgery, and stereotactic radiosurgery, providing comprehensive diagnosis and treatment for various neurosurgical diseases such as brain and spinal cord tumors, cerebrovascular diseases, and craniocerebral injuries.
Renji Hospital Affiliated to Shanghai Jiao Tong University School of Medicine

https://www.shsmu.edu.cn/ylfw/fsyy1/fsrjyy.htm
– Department Strength: Founded in 1956, it is a National Clinical Key Specialty under the Ministry of Health. The clinical department has 155 beds, with 40,000 outpatient visits and over 3,300 surgeries annually. It has rich experience in microsurgical and endoscopic techniques for brain tumors, as well as comprehensive treatment of cerebrovascular diseases.
– Specialties: Sub-specialties include endoscopic minimally invasive surgery, cerebrovascular diseases, supratentorial and infratentorial tumors, spinal cord and spine surgery, craniocerebral trauma and critical care, and pediatric neurosurgery.
Ruijin Hospital, Shanghai Jiao Tong University School of Medicine

https://www.rjh.com.cn
The Department of Neurosurgery at Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, is a renowned medical specialty with nearly half a century of development. As a national training base for neurosurgical specialists and a neuroendoscopy training center, it boasts advanced facilities like DSA hybrid operating rooms and intraoperative navigation systems.
Its main strengths are in performing minimally invasive surgeries for brain tumors, providing standardized care for pituitary adenomas (with over 200 surgeries each year and a remission rate of more than 90% for Cushing’s disease), and using new “zero-traction” methods in microvascular decompression for nerve issues. With a team of 29 physicians, including 18 senior experts, it integrates multidisciplinary approaches to provide precise and personalized care.
Beijing
Beijing Tiantan Hospital Affiliated to Capital Medical University

Department Strength: Ranked 1st in the 2022 neurosurgery specialty comprehensive ranking, it is the largest neurosurgical clinical, teaching, and research center in China with the most complete sub-specialties. It is a key discipline of the Ministry of Education, a key specialty of the Ministry of Health, and a “National Clinical Research Center for Neurological Diseases.” The elective surgery mortality rate is 0.16%, reaching an internationally advanced level.
Specialties: The hospital has 21 departments that focus on brain and spine issues, including strokes, children’s brain surgery, head injuries, spinal problems, and certain brain tumors, and it is a leader globally in treating specific types of brain and blood vessel conditions.
Xuanwu Hospital Affiliated to Capital Medical University
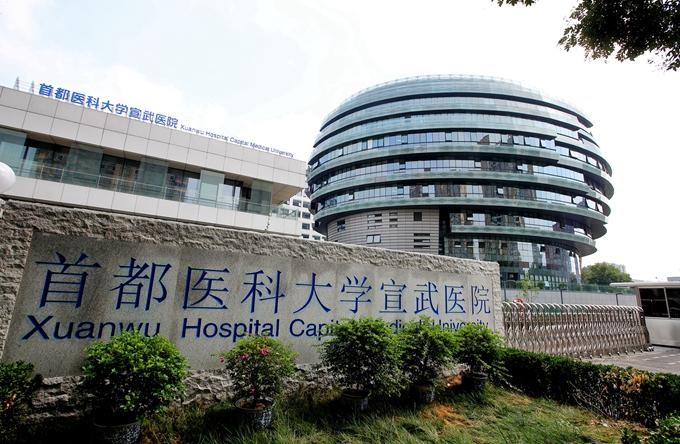
Department Strength: Ranked 4th in the 2022 neurosurgery specialty comprehensive ranking, it is a National Medical Center for Neurological Diseases and one of the first national clinical key specialties. The neurosurgery department has a total of 345 beds, performing over 10,000 neurosurgical operations annually.
Specialties: It has established 10 sub-specialty groups, including a cerebrospinal vascular disease center, a cerebral revascularization center, and a neurospine center, providing high-quality diagnosis and treatment for various complex neurological diseases.
Chinese People’s Liberation Army General Hospital (Beijing 301 Hospital)

https://www.301hospital.com.cn/index.html
Department Strength: Ranked 7th in the 2022 neurosurgery specialty comprehensive ranking, this department is recognized as a national clinical key specialty and serves as the PLA Neurosurgery Institute, which is the largest and most renowned neurosurgical center in the PLA, performing nearly 20,000 surgeries annually. Its research on “moyamoya disease” is at the international advanced level, and it was the first in China to carry out advanced techniques such as deep hypothermic circulatory arrest for complex intracranial aneurysms.
Specialties: The department has six sub-specialties, including craniocerebral trauma surgery, neuro-oncology surgery, and cerebrovascular surgery, specializing in the diagnosis and treatment of cerebrovascular diseases, skull base and deep brain tumors, pituitary adenomas, and other diseases.
Dr. Nishant Mittal is a highly accomplished researcher with over 13 years of experience in the fields of cardiovascular biology and cancer research. His career is marked by significant contributions to stem cell biology, developmental biology, and innovative research techniques.
Research Highlights
Dr. Mittal's research has focused on several key areas:
1) Cardiovascular Development and Regeneration: He studied coronary vessel development and regeneration using zebrafish models1.
2) Cancer Biology: At Dartmouth College, he developed zebrafish models for studying tumor heterogeneity and clonal evolution in pancreatic cancer.
3) Developmental Biology: His doctoral work at Keio University involved identifying and characterizing medaka fish mutants with cardiovascular defects.
4) Stem Cell Research: He investigated the effects of folic acid on mouse embryonic stem cells and worked on cryopreservation techniques for hematopoietic stem cells.
Publications and Presentations
Dr. Mittal has authored several peer-reviewed publications in reputable journals such as Scientific Reports, Cardiovascular Research, and Disease Models & Mechanisms1. He has also presented his research at numerous international conferences, including the Stanford-Weill Cornell Cardiovascular Research Symposium and the Weinstein Cardiovascular Development Conference.
In summary, Dr. Nishant Mittal is a dedicated and accomplished researcher with a strong track record in cardiovascular and cancer biology, demonstrating expertise in various model systems and a commitment to advancing scientific knowledge through innovative research approaches.
- Nishant Mittal (PhD)https://cancerfax.com/author/nishantm/
- Nishant Mittal (PhD)https://cancerfax.com/author/nishantm/
- Nishant Mittal (PhD)https://cancerfax.com/author/nishantm/
- Nishant Mittal (PhD)https://cancerfax.com/author/nishantm/
Related Posts
- Comments Closed
- June 2nd, 2025


- Datopotamab deruxtecan-dlnk is approved by the USFDA for EGFR-mutated non-small cell lung cancer
- Tafasitamab-cxix is approved by the USFDA for relapsed or refractory follicular lymphoma
- PiggyBac Transposon System: A Revolutionary Tool in Cancer Gene Therapy
- Breakthrough Treatments for Advanced Breast Cancer in 2025
- Neoadjuvant and adjuvant pembrolizumab is approved by the USFDA for resectable locally advanced head and neck squamous cell carcinoma
- Mitomycin intravesical solution is approved by the USFDA for recurrent low-grade intermediate-risk non-muscle invasive bladder cancer
- Taletrectinib is approved by the USFDA for ROS1-positive non-small cell lung cancer
- Darolutamide is approved by the USFDA for metastatic castration-sensitive prostate cancer
- Atezolizumab Plus Chemotherapy Improves Survival in Advanced-Stage Small-Cell Lung Cancer: Insights from the IMpower133 Study
- Satri-cel CAR T-Cell Therapy: A New Era in Gastric Cancer Treatment
- AI & Technology (12)
- Aids cancer (4)
- Anal cancer (9)
- Appendix cancer (3)
- Basal cell carcinoma (1)
- Bile duct cancer (7)
- Biotech Innovations (19)
- Bladder cancer (12)
- Blood cancer (60)
- Bone cancer (12)
- Bone marrow transplant (47)
- Brain Cancer (1)
- Breakthrough Research (17)
- Breast Cancer (53)
- Cancer Guides (10)
- Cancer News and Updates (54)
- Cancer Treatment Abroad (286)
- Cancer treatment in China (316)
- Cancer Treatments (12)
- Cancer Types (5)
- Cancer Warriors (1)
- CAR T Protocols (2)
- CAR T-Cell therapy (135)
- Cervical cancer (40)
- Chemotherapy (55)
- Childhood cancer (2)
- Cholangiocarcinoma (3)
- Clinical trials (15)
- Colon cancer (96)
- Diagnosis & Staging (4)
- Doctors & Researchers (76)
- Drug Approvals (100)
- Drugs (80)
- Endometrial cancer (10)
- Esophageal cancer (15)
- Eye cancer (9)
- For Doctors and Researchers (12)
- Gall bladder cancer (3)
- Gastric cancer (29)
- Gene therapy (5)
- Glioblastoma (7)
- Glioma (10)
- Global Trial News (5)
- Gynecological cancer (2)
- Head and neck cancer (19)
- Hemato-Oncologist (1)
- Hematological Disorders (52)
- Hospital Reviews (3)
- How to Participate (6)
- Immunotherapy (34)
- Kidney cancer (10)
- Laryngeal cancer (1)
- Leukemia (49)
- Liver cancer (101)
- Lung cancer (82)
- Lymphoma (52)
- MDS (2)
- Melanoma (9)
- Merkel cell carcinoma (1)
- Mesothelioma (5)
- Myeloma (25)
- Myths vs Facts (5)
- Neuroblastoma (7)
- NK-Cell therapy (13)
- Nutrition (1)
- Ongoing Trials (11)
- Oral cancer (12)
- Ovarian Cancer (14)
- Pancreatic cancer (43)
- Paraganglioma (6)
- Patient Testimonials (1)
- Penile cancer (1)
- Prostrate cancer (11)
- Proton therapy (28)
- Radiotherapy (56)
- Recovery Tips (2)
- Rectal cancer (58)
- Research Insights (8)
- Sarcoma (14)
- Skin Cancer (13)
- Spine surgery (24)
- Stomach cancer (40)
- Success Stories (1)
- Surgery (102)
- Systemic mastocytosis (1)
- T Cell immunotherapy (7)
- Targeted therapy (9)
- Testicular cancer (5)
- Thoracic surgery (2)
- Throat cancer (6)
- Thyroid Cancer (15)
- Treatment Cost (1)
- Treatment in China (969)
- Treatment in India (1,273)
- Treatment in Israel (652)
- Treatment in Malaysia (425)
- Treatment in Singapore (321)
- Treatment in South Korea (305)
- Treatment in Thailand (291)
- Treatment in Turkey (272)
- Treatment Planning (151)
- Trial Results (2)
- Uncategorized (105)
- Urethral cancer (9)
- Urosurgery (14)
- Uterine cancer (4)
- Vaginal cancer (6)
- Vascular cancer (5)
- Vulvar cancer (1)

brain glioma treatment China, CAR-T therapy brain cancer, glioblastoma therapy China, glioma clinical trials China, glioma research China, glioma survival rate China, glioma treatment guidelines China, immunotherapy for glioma, ONC201 glioma China, targeted therapy glioma China
CancerFax is the most trusted online platform dedicated to connecting individuals facing advanced-stage cancer with groundbreaking cell therapies.
Send your medical reports and get a free analysis.
🌟 Join us in the fight against cancer! 🌟
Привет,
CancerFax — это самая надежная онлайн-платформа, призванная предоставить людям, столкнувшимся с раком на поздних стадиях, доступ к революционным клеточным методам лечения.
Отправьте свои медицинские заключения и получите бесплатный анализ.
🌟 Присоединяйтесь к нам в борьбе с раком! 🌟