
Cancer Vaccines
A cancer vaccine is a new kind of medicine that uses the body’s immune system to try to avoid or treat cancer. Cancer vaccines are different from other vaccines because they don’t protect against illnesses. Instead, they cause the immune system to attack tumour cells. They can be grouped into two main types: preventive and therapeutic. Preventive vaccines help stop cancer from happening by attacking viruses or other factors linked to cancer.
Therapeutic vaccines help treat cancer by making the immune system better able to recognize and attack cancer cells. These hopeful vaccines give people hope for a future in which cancer rates go down and survival rates go up. They also open up new ways to treat and get rid of cancer.
What is cancer vaccine?
A cancer vaccine is a new medical method that uses the body’s immune system to fight cancer. Cancer vaccines are different from other vaccines because they don’t protect against infectious diseases. Instead, they work by getting the immune system to attack cancer cells. The main goal of a cancer vaccine is to either stop cancer from happening or to treat cancer that has already started. This is done by making the immune system better able to find and fight cancerous cells.
There are two main kinds of cancer vaccines: ones that avoid cancer and ones that treat cancer. Vaccines that prevent cancer try to protect against viruses or other things that can cause cancer or make it worse. On the other hand, therapeutic vaccines are meant to treat existing cancers by teaching the immune system to recognise and target specific tumour proteins.
Even though cancer vaccines have a lot of potential, their development and success depend on the type of cancer being fought and how each person’s immune system reacts. Immunology study is still going on and making progress, which gives us hope for more progress in the fight against cancer through vaccines.
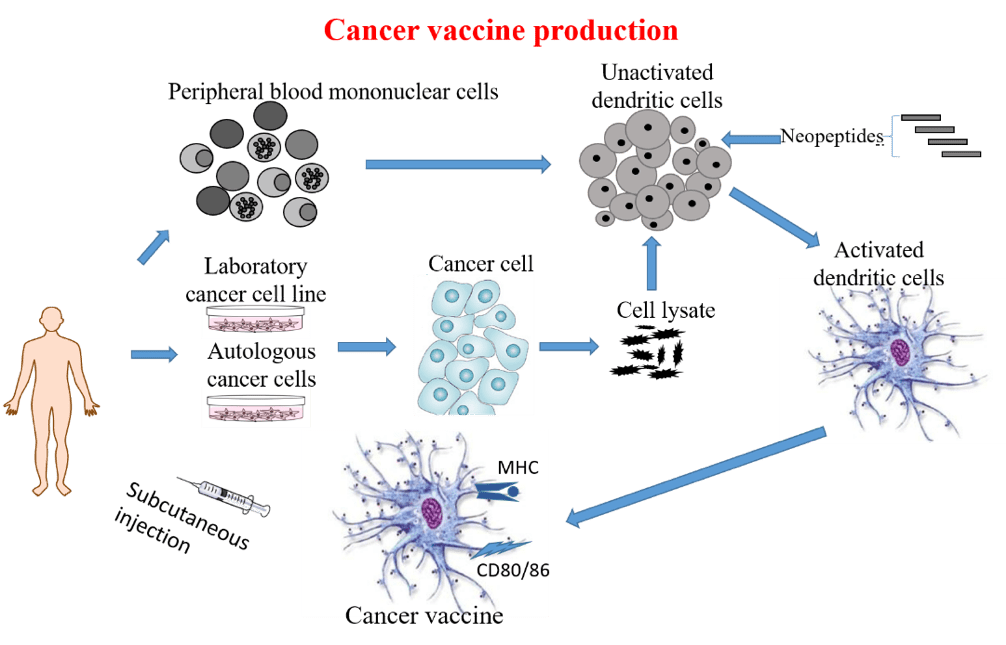
Tumour antigens are pieces of proteins made by cancer cells that have changed their genes. Many of them look like normal proteins, so the immune system can’t tell them apart. Many tumour vaccines are based on a single tumour antigen, while others use tumour lysates or peptides to base their vaccines on more than one antigen. Neoantigens, which are new antigens made from tumour mutations and based on whole exome sequencing (WES), have been looked at as possible new cancer medicines. Dendritic-cell-based cancer vaccines change the immune system by using dendritic cells that have been changed genetically to prime and trigger T cells so they can attack cancer cells. The second is a more advanced method of making a cancer vaccine, but it is harder to design and use.
How cancer vaccine are produced?
How cancer vaccine work?
The autoimmune response is activated to target cancer cells
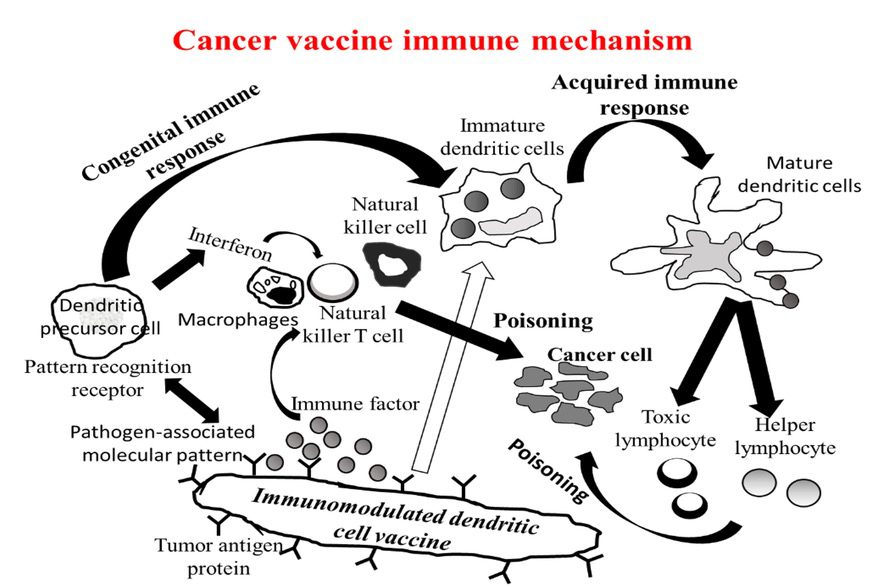
Cancer cells arise everyday and are eliminated all the time by our immune system. When the immune function is compromised, or sometimes, severe cancer mutations occur by chance, the cancer cells may breakthrough the immune surveillance. Therefore, the activation and enhancement of the immune system to recognize cancer cells is important for treating cancer.
To improve and enhance the immune reactivity of cancer vaccines
Traditional vaccines are based on weakened or inactivated viruses or bacteria that may trigger an immune response in the body. Tumor vaccine development has evolved from the early generation of whole tumor lysates to the current neopeptide tumor vaccines.
Immunologically modified dendritic cells
Cancer vaccine uses the latest technology to include immune gene modified tumors and DCs to present multiple tumor antigens, as well as to synthesize new tumor mutation peptides (neoepitopes) via NGS WES and computer-aided HLA restricted epitope prediction technology. The immune gene modified dendritic cell vaccines enhance presentation of specific cancer antigens, which at the same time produce immune-stimulating factors, promoting the immune system to recognize cancer cells. Including natural killer cells and dendritic cells in the immune system, theyy trigger a strong anticancer response, and induce cytotoxic T lymphocytes to kill cancer cells.
Cancer vaccine can induce memory T lymphocytes
Cancer vaccines can prevent cancer recurrence and metastasis. Surgery, chemotherapy or radiotherapy can remove most of the tumors, yet, there are still residual cancer cells, which may lead to recurrence and metastasis. GIMI immune modulation technologyy is based on gene modifiedd DC-based cancer vaccine that can induce memory-type T-lymphocytes, and attack cancer cells. In other words, it can prevent cancer recurrence or metastasis after the cancer vaccine is administered.
NeoP VAX Vaccine
The analysis originates from neoepitope prediction based on the patient’s tumor sequencing data. A tumor sample is obtained by a biopsy. Then, genes and variants that are expressed in the tumor sample of the patient are chosen and made even better so that a stable and effective peptide is made. The sequences that correspond to peptides that would best bind to different HLA class I and II molecules are prioritized for synthesis.
PanAM VAX Vaccine
The PanAm VAX vaccine is a peptide-based vaccine with a singular purpose, to help the immune system identify markers specific to blood vessels that feed tumors.
While it is an off-the-shelf product, the peptides used in the production of this vaccine are found in around 98% of all tumor-related blood vessels, making it an efficient way to help diminish blood flow, and inhibiting a tumor’s ability to protect itself from the immune system.
In cutting off a tumor’s blood supply, it will undergo oxidative stress and become more susceptible to attack by the immune system due to its weakened state.
CellX Vaccine
This proprietary placenta-derived vaccine affords us the ability to train the immune system to recognize and selectively destroy tumor blood vessels exclusively. This is a second-generation vaccine that has undergone rigorous clinical testing and has shown to be effective in a variety of solid tumor applications.
Cervical cancer vaccine
The HPV vaccine, which protects against cervical cancer, is a very important medical development in the fight against cervical cancer. Human papillomavirus (HPV) is a common sexually spread infection that can cause cervical cancer. The vaccine protects against the most dangerous types of HPV, which are the cause of most cases of cervical cancer.
The vaccine is usually given as a set of shots over a few months. It works best when given before a person starts having sexual relations. It is recommended for both men and women to help stop the spread of HPV and lower the number of people who have the virus generally.
One of the best things about the cervical cancer vaccine is that it could make cervical cancer, which is the fourth most common cancer in women worldwide, much less common. By preventing HPV infection, the vaccine could save thousands of lives each year and make it easier for health services around the world to deal with cervical cancer.
Also, a lot of clinical studies and use in the real world have shown that the vaccine is safe and works. Because it worked so well, many countries have started programmes to give the vaccine to young people. This has made it even better for public health.
In conclusion, the cervical cancer vaccine is an effective way to fight cervical cancer and other diseases caused by HPV. By preventing HPV infection, it is a key factor in lowering the number of cervical cancer cases and making the world’s health better generally. To make the most of the vaccine and protect future generations from the terrible effects of cervical cancer, people need to know about it and be able to get it.
Lung cancer vaccines: Cimavax and Vaxira
Both CimaVax and Vaxira are experimental vaccines that have been looked at to see if they could be used to treat lung cancer.

CimaVax is a treatment vaccine for lung cancer that was made in Cuba. CimaVax is different from other vaccines because it tries to get the immune system to make antibodies against a protein called epidermal growth factor (EGF). EGF helps cells grow and also plays a role in how cancer starts and spreads. By going after EGF, CimaVax hopes to stop lung cancer cells from growing and spreading. This could help people with advanced lung cancer live longer.
On the other hand, Vaxira is a vaccine against cancer that was made in Argentina. It goes after a different protein called MUC1, which is overproduced in lung cancer and other types of cancer. Vaxira is meant to get the immune system to recognise MUC1-expressing cancer cells and fight them.
Both CimaVax and Vaxira are promising research directions in the area of treating lung cancer.

Clinical trials have shown promising results, and more study is being done to find out how well they work over time and if they could be used as part of a full lung cancer treatment plan. As of my last knowledge update in September 2021, these vaccines were still being researched, and their access and use may have changed since then. Always talk to a doctor or nurse for the most up-to-date advice on how to treat lung cancer.
Where is cancer vaccine available now?
Cancer vaccine produced by dendritic methods is available in China. Those who are interested to get themselves vaccinated against cancer can avail the therapy. Those patients who are diagnosed with cancer can also take the vaccine. Cimavax is available in Cuba whereas Vaxira is available in Argentina at present.
As of my last report, which was in June 2023, there were not many cancer vaccines available, and most of the work in the field was still in the research and development stage. There were some vaccines to prevent cancer, like the Human Papillomavirus (HPV) vaccine to prevent cervical cancer and other cancers, and the Hepatitis B vaccine to lower the risk of liver cancer. However, these vaccines were aimed at specific viruses that cause cancer, not cancer cells directly.
Therapeutic cancer vaccines, which are meant to treat cancers that have already started, were still being tested in clinical studies for different types of cancer. These studies were important for figuring out if they were safe, if they worked, and if they could cause any side effects. Cancer vaccines were hard to make because it was hard to find the right tumour antigens, make medicines fit each patient, and figure out how to stop cancer from hiding from the immune system.
It’s important to remember that the field of medical study and the treatments that are available may have changed since my last update. For the most up-to-date information on cancer vaccines and other treatments, it is best to talk to current medical sources and healthcare workers.
What is the cost of cancer vaccines?
Dendritic cell based vaccines cost around $ 22000 USD. The course of treatment for Vaxira, which consists of five buildup shots given every two weeks and then ten booster shots given every four weeks, costs around $25,000.
Cervical cancer vaccine will cost around $ 100 USD per dose. Cervical cancer vaccine that is made by Serum Institute of India is suppose to be costing less than $ 10USD per dose.