Atezolizumab plus Bevacizumab for treatment of liver cancer
July 13th 2021: A novel medication for people with a kind of liver cancer called hepatocellular carcinoma is available that appears to be better than standard therapy (HCC). The Food and Drug Administration (FDA) approved atezolizumab (Tecentriq) and bevacizumab (Avastin) as first-line treatments for persons with advanced liver cancer who cannot be treated surgically.
Patients with liver cancer treated with Atezolizumab with Bevacizumab lived significantly longer than those treated with sorafenib in the IMbrave150 study that resulted to the approval (Nexavar). They were also able to live longer without their cancer progressing. The outcomes of the study were published in the New England Journal of Medicine on May 14th.
One of the study’s experts, Richard Finn, M.D., of the University of California, Los Angeles, said, “This is a major advance for patients.” “This is something that clinicians who treat these patients have been asking for for a long time, and it is a huge step forward.”
Atezolizumab is an immune checkpoint inhibitor, which means it helps the immune system find and kill cancer cells. Bevacizumab is a targeted medication that starves tumours by inhibiting the growth of new blood vessels.
Another targeted therapy, sorafenib, inhibits the formation of blood vessels and cancer cells. Sorafenib was the first medicine approved by the FDA in 2007 to treat certain HCC patients.
According to Tim Greten, M.D., deputy chief of the NCI’s Center for Cancer Research’s Thoracic and GI Malignancies Branch, the only therapies for HCC that have been licenced since 2007 are no more effective than sorafenib.
In an editorial, Robin Kelley, M.D., of the UCSF Helen Diller Family Comprehensive Cancer Center, stated that not only was the atezolizumab–bevacizumab combination more effective, but it also resulted in “strikingly better patient-reported outcomes,” such as physical capacities.
According to Dr. Greten, the combo regimen will likely replace sorafenib as the usual first-line treatment for some persons with advanced HCC.
Adding to immune checkpoint inhibitors
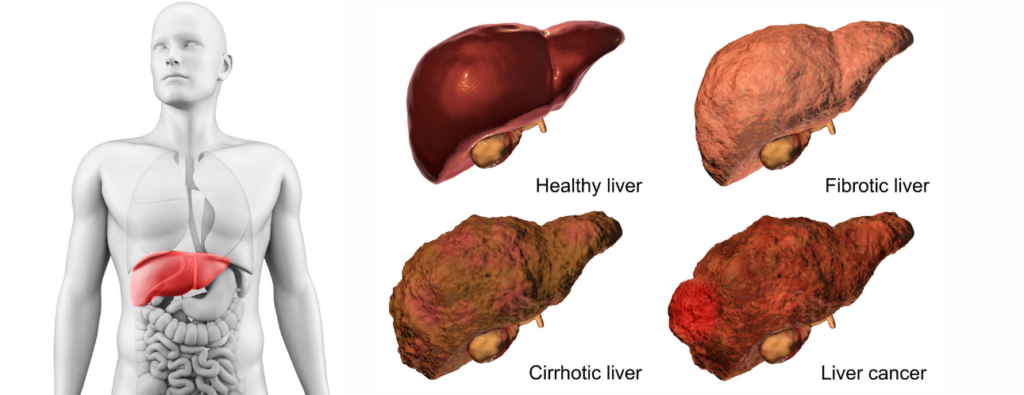
Liver cancer is frequently identified after it has progressed outside the liver or become interwoven with several blood arteries, making surgery impossible to treat.
Sorafenib and lenvatinib (Lenvima), another medicine that slows blood vessel formation, are the sole options for persons with liver cancer who can’t be treated with surgery (is inoperable).
Immune checkpoint inhibitors were explored as first-line therapies for liver cancer in a few clinical studies, but they were found to be ineffective on their own. Scientists discovered that excessive amounts of a protein called VEGF may hinder immune checkpoint drugs from working after further investigation.
According to Dr. Finn, VEGF induces the creation of new blood vessels and alters the quantity and type of immune system cells in and around tumours.
Because bevacizumab inhibits VEGF, researchers from Genentech and a number of medical institutions compared atezolizumab to bevacizumab in a limited study of patients with liver cancer. They reported in 2019 that the combination was more successful than atezolizumab alone and had manageable adverse effects. The IMbrave150 study is a follow-up to the previous one.
Safety of Atezolizumab Plus Bevacizumab
The combo medication caused several negative effects in many patients. Overall, though, patients appeared to tolerate both medicines, according to Dr. Greten.
The two groups had equal incidence of side effects and fatalities from side effects. However, the combo group had more patients who experienced any major adverse effects (38 percent versus 31 percent ).
Because of side effects, fewer patients in the combo group paused or modified the dose of their therapy (50 percent versus 61 percent in the sorafenib group). Only 7% of patients in the combination group stopped taking both medications due to adverse effects, despite the fact that more patients in the combination group stopped taking one of the drugs (16% versus 10%).
Because of its impact on blood arteries, bevacizumab can cause bleeding, according to Dr. Greten. He stated that liver cancer can also create changes that increase the risk of bleeding, such as low platelet counts.
“There were a few more bleeding episodes in the atezolizumab, bevacizumab arm, but they were still very low as a percentage,” Dr. Finn added. In both groups, 6% of patients experienced significant bleeding as a result of bevacizumab treatment.
According to Dr. Greten, “it will be critical to select the suitable patient population” for the combo treatment. Before starting the medication, patients may need to obtain standard tests to check for bleeding risk factors, he said.
Dr. Kelley said, “Alternative therapy should be investigated for patients at high risk of bleeding.”
- Comments Closed
- July 13th, 2021


Latest drugs
CancerFax is the most trusted online platform dedicated to connecting individuals facing advanced-stage cancer with groundbreaking cell therapies.
Send your medical reports and get a free analysis.
🌟 Join us in the fight against cancer! 🌟
Привет,
CancerFax — это самая надежная онлайн-платформа, призванная предоставить людям, столкнувшимся с раком на поздних стадиях, доступ к революционным клеточным методам лечения.
Отправьте свои медицинские заключения и получите бесплатный анализ.
🌟 Присоединяйтесь к нам в борьбе с раком! 🌟