Oral Cancer Radiotherapy
Introduction
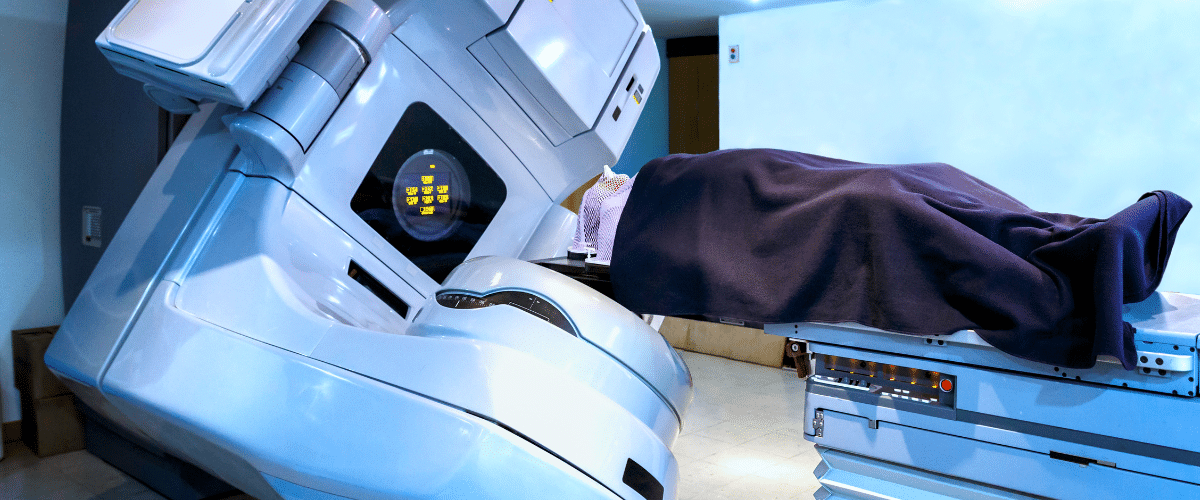
Radiotherapy for oral cancer is a treatment mainstay in most patients with mouth and oropharyngeal cancers. Radiotherapy employs high-energy beams to kill cancer cells, and in most cases, it is either a first-line therapy or used with surgery and chemotherapy. This in-depth blog discusses the application of radiotherapy for oral cancer treatment, encompassing modalities, efficacy, medications employed, economic costs, and accessibility in India and China.
About the Disease
Oral cancer is cancer that occurs in the lips, tongue, cheeks, floor of the mouth, hard and soft palate, and throat. It is a head and neck cancer subtype, with the most common being squamous cell carcinoma. Risk factors are tobacco and alcohol consumption, poor oral hygiene, HPV infection, and long sun exposure (for lip cancer).
Oral cancer tends to be diagnosed late because the early symptoms are not very prominent. The success of treatment depends mainly on early diagnosis, and radiotherapy is an important factor in both early and advanced disease.
Indications for Radiotherapy in Oral Cancer
Radiotherapy is indicated in various clinical situations for oral cancer patients:
-
Primary treatment for early-stage cancer (especially when surgery isn’t preferred)
-
Adjuvant therapy after surgery to destroy residual cancer cells
-
Neoadjuvant therapy in combination with chemotherapy
-
Definitive chemoradiotherapy in locally advanced tumors
-
Palliative radiotherapy to relieve symptoms in metastatic cancer
You can use it alone or in combination with chemotherapy (concurrent chemoradiotherapy), especially for inoperable or locally advanced tumors.
Treatment Details
Typically, a series of daily sessions, or fractions, delivers radiotherapy for oral cancer over several weeks. Treatment planning includes imaging (CT/MRI) and mapping of tumor volume using advanced techniques.
Types of Radiotherapy:
-
External Beam Radiotherapy (EBRT): The most common form. Delivered via:
-
Intensity-Modulated Radiation Therapy (IMRT)
-
Image-Guided Radiation Therapy (IGRT)
-
3D Conformal Radiation Therapy (3D-CRT)
-
-
Brachytherapy: Internal radiotherapy using radioactive implants placed near the tumor (less common in oral cancers but effective in selected cases).
Radiotherapy Duration:
-
Typically, 5 days a week for 6–7 weeks.
-
Total dose ranges from 60 to 70 Gy depending on the disease stage.
Medicines Used During Radiotherapy
While radiation itself is a physical treatment, certain medications are used concurrently or as supportive care:
Radiosensitizers:
-
Cisplatin – Enhances radiation efficacy, commonly used weekly.
-
Fluorouracil (5-FU) – Sometimes used with Cisplatin or Capecitabine.
-
Cetuximab – A monoclonal antibody used in targeted radiotherapy for patients unfit for Cisplatin.
Supportive Drugs:
-
Anti-nausea medications (Ondansetron, Granisetron)
-
Pain relief (NSAIDs, opioids)
-
Mouth rinses and oral gels (to manage mucositis)
-
Nutritional supplements
-
Antibiotics/antifungals (for oral infections)
Effectiveness of Radiotherapy
Radiotherapy is highly effective, especially in early-stage cancers or as an adjunct to surgery. Key outcomes include:
-
Early-stage tumors: Cure rates of up to 85%
-
Locally advanced disease: 40-60% disease control with chemoradiotherapy
-
Palliative setting: Significant symptom relief in over 70% of patients
IMRT and IGRT have improved precision, reducing side effects while preserving nearby healthy tissue.
Risks and Side Effects
Radiotherapy, while effective, can cause both acute and long-term side effects due to the sensitivity of oral tissues.
Common Acute Side Effects:
-
Oral mucositis (painful mouth sores)
-
Dry mouth (xerostomia)
-
Difficulty swallowing (dysphagia)
-
Fatigue
-
Changes in taste
-
Skin reactions in the treated area
Long-term Side Effects:
-
Chronic dry mouth
-
Tooth decay and jaw stiffness (osteoradionecrosis)
-
Speech and swallowing difficulties
-
Hypothyroidism (if neck region is irradiated)
Oral care during treatment is essential to minimize complications.
Recovery and Aftercare
Post-radiotherapy recovery requires comprehensive aftercare focused on restoring oral function, managing side effects, and monitoring for recurrence.
Aftercare Components:
-
Regular follow-up every 1–3 months in the first year
-
Dental care with fluoride treatments
-
Speech and swallowing therapy
-
Nutritional support (high-protein, soft foods)
-
Smoking and alcohol cessation
-
Psychological support and rehabilitation
Healing may take several weeks to months after completing therapy.
Cost and Availability
Radiotherapy cost depends on the technique used (IMRT vs 3D-CRT), hospital location, and whether the patient is in a government or private facility.
In India:
-
3D-CRT: ₹30,000 – ₹60,000 (USD 350 – 700)
-
IMRT: ₹1,00,000 – ₹2,50,000 (USD 1,200 – 3,000)
-
Available in major cancer centers like Tata Memorial, AIIMS, and Apollo
In China:
-
Public hospitals offer basic radiotherapy at ¥8,000 – ¥15,000 per course
-
IMRT and IGRT: ¥25,000 – ¥60,000 (USD 3,000 – 8,000)
-
Advanced centers like Fudan University Cancer Hospital and Peking Union Medical College Hospital provide high-end radiotherapy
Both countries are investing in expanding radiotherapy units, especially in tier-2 and tier-3 cities.
Patient Experiences
Patients undergoing oral cancer radiotherapy report both physical and emotional challenges during treatment. However, with adequate preparation and supportive care, most patients complete therapy successfully.
Common feedback includes:
-
Painful mouth sores during weeks 3–5
-
Difficulty eating and weight loss
-
Relief and satisfaction after tumor shrinkage
-
Emotional highs during recovery and regaining speech/swallowing abilities
Many patients highlight the importance of patient education, hydration, and supportive counseling.
Cost in Countries (in USD)
| Country | 3D-CRT Radiotherapy | IMRT / IGRT | Targeted Chemoradiotherapy |
|---|---|---|---|
| China | $1,000 – $2,200 | $3,000 – $8,000 | $6,000 – $12,000 |
| India | $400 – $700 | $1,200 – $3,000 | $3,000 – $6,000 |
| Israel | $4,000 – $7,000 | $7,000 – $14,000 | $10,000 – $18,000 |
| Malaysia | $1,500 – $3,000 | $4,000 – $6,000 | $7,000 – $12,000 |
| South Korea | $3,000 – $6,000 | $7,000 – $10,000 | $10,000 – $15,000 |
| Thailand | $1,200 – $2,800 | $3,000 – $6,000 | $5,000 – $9,000 |
| Turkey | $1,500 – $4,000 | $4,000 – $8,000 | $7,000 – $10,000 |
| USA | $7,000 – $15,000 | $15,000 – $30,000 | $25,000 – $45,000 |
List of Ongoing Clinical Trials in China
Several clinical trials are underway in China to improve radiotherapy for oral cancer:
-
Proton therapy trials for oral and oropharyngeal carcinoma (Shanghai Proton Center)
-
IMRT combined with immunotherapy for locally advanced oral cancers
-
Evaluation of radiation-induced gene expression markers for predicting response
-
Brachytherapy vs external beam radiation comparison in early-stage lip cancer
-
Photodynamic therapy adjunct with radiotherapy in recurrent tumors
Chinese cancer centers are actively integrating AI and imaging tools into radiation planning for improved accuracy.
FAQ
How is radiotherapy delivered for oral cancer?
Usually via external beam radiation (EBRT), with IMRT being the most common technique.
How long does radiotherapy take?
It typically takes 6 to 7 weeks, with 30–35 sessions.
Is radiotherapy painful?
The procedure itself is painless, but side effects such as mouth sores and dry mouth can be painful.
What should I eat during radiotherapy?
Soft, bland, high-protein foods. Avoid spicy, hard, or acidic foods. Hydration is critical.
Can radiotherapy cure oral cancer?
Yes, particularly in early stages. In advanced cases, it controls disease and relieves symptoms.
What is the role of IMRT?
IMRT precisely targets tumors while minimizing damage to surrounding healthy tissue.
Can radiotherapy be repeated if cancer returns?
Re-irradiation is sometimes possible but depends on prior dose and location.
Is radiotherapy available in Indian and Chinese government hospitals?
Yes, both offer radiotherapy in regional and national cancer centers at subsidized rates.