Liver cancer
About Disease
Liver cancer is the growth and spread of unhealthy cells in the liver. Cancer that starts in the liver is called primary liver cancer. Cancer that spreads to the liver from another organ is called metastatic liver cancer. Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer.
Liver
The liver is made up of cells called hepatocytes. It also has other types of cells, including cells that line its blood vessels and cells that line small tubes in the liver called bile ducts. The bile ducts carry bile from the liver to the gallbladder or directly to the intestines.
The liver is the largest glandular organ in the body and performs various critical functions to keep the body free of toxins and harmful substances. It’s located in the right upper quadrant of the abdomen, right below the ribs. The liver is responsible for producing bile, which is a substance that helps you digest fats, vitamins, and other nutrients.
This vital organ also stores nutrients such as glucose so that you remain nourished at times when you’re not eating. It also breaks down medications and toxins. When cancer develops in the liver, it destroys liver cells and interferes with the ability of the liver to function normally.
Liver cancer is generally classified as primary or secondary. Primary liver cancer begins in the cells of the liver. Secondary liver cancer develops when cancer cells from another organ spread to the liver. Unlike other cells in the body, cancer cells can break away from the primary site, or where the cancer began. The cells travel to other areas of the body through the bloodstream or the lymphatic system. Cancer cells eventually collect in another body organ and begin to grow there.
You cannot live without your liver. It has many important functions:
- It breaks down and stores many of the nutrients absorbed from the intestine that your body needs to function. Some nutrients must be changed (metabolized) in the liver before they can be used for energy or to build and repair body tissues.
- It makes most of the clotting factors that keep you from bleeding too much when you are cut or injured.
- It delivers bile into the intestines to help absorb nutrients (especially fats).
- It breaks down alcohol, drugs, and toxic wastes in the blood, which then pass from the body through urine and stool
The different types of cells in the liver can form several types of malignant (cancerous) and benign (non-cancerous) tumors. These tumors have different causes, are treated differently, and have a different prognosis (outlook).
Types of liver cancer
Primary liver cancer
A cancer that starts in the liver is called primary liver cancer. There is more than one kind of primary liver cancer.
Hepatocellular carcinoma (HCC)
This condition is the most common form of liver cancer in adults.
Hepatocellular cancers can have different growth patterns:
- Some begin as a single tumor that grows larger. Only late in the disease does it spread to other parts of the liver.
- A second type seems to start as many small cancer nodules throughout the liver, not just a single tumor. This is seen most often in people with cirrhosis (chronic liver damage) and is the most common pattern seen in the United States.
Doctors can classify several subtypes of HCC. Most often these subtypes do not affect treatment or prognosis (outlook). But one of these subtypes, fibrolamellar, is important to recognize. It is rare, making up less than 1% of HCCs, and is most often seen in women younger than age 35. Often the rest of the liver is not diseased. This subtype tends to havea better outlook than other forms of HCC.
Intrahepatic cholangiocarcinoma (bile duct cancer)
About 10% to 20% of cancers that start in the liver are intrahepatic cholangiocarcinomas. These cancers start in the cells that line the small bile ducts (tubes that carry bile to the gallbladder) within the liver. Most cholangiocarcinomas, however, actually start in the bile ducts outside the liver.
Although the rest of this information is mainly about hepatocellular cancers, cholangiocarcinomas are often treated the same way. For more detailed information on this type of cancer, see Bile Duct Cancer.
Angiosarcoma and hemangiosarcoma
These are rare cancers that begin in cells lining the blood vessels of the liver. People who have been exposed to vinyl chloride or to thorium dioxide (Thorotrast) are more likely to develop these cancers. Some other cases are thought to be caused by exposure to arsenic or radium, or to an inherited condition known as hereditary hemochromatosis. In about half of all cases, no likely cause can be identified.
These tumors grow quickly and are usually too widespread to be removed surgically by the time they are found. Chemotherapy and radiation therapy may help slow the disease, but these cancers are usually very difficult to treat. These cancers are treated like other sarcomas. For more information, see Soft Tissue Sarcoma.
Hepatoblastoma
This is a very rare kind of cancer that develops in children, usually in those younger than 4 years old. The cells of hepatoblastoma are similar to fetal liver cells. About 2 out of 3 children with these tumors are treated successfully with surgery and chemotherapy, although the tumors are harder to treat if they have spread outside the liver.
Secondary liver cancer (metastatic liver cancer)
Most of the time when cancer is found in the liver, it did not start there but has spread (metastasized) from somewhere else in the body, such as the pancreas, colon, stomach, breast, or lung. Because this cancer has spread from its original (primary) site, it is called a secondary liver cancer. These tumors are named and treated based on their primary site (where they started). For example, cancer that started in the lung and spread to the liver is called lung cancer with spread to the liver, not liver cancer. It is also treated as lung cancer.
In the United States and Europe, secondary (metastatic) liver tumors are more common than primary liver cancer. The opposite is true for many areas of Asia and Africa.
For more information on liver metastases from different types of cancer, see specific cancer types, as well as Advanced Cancer.
Benign liver tumors
Benign tumors sometimes grow large enough to cause problems, but they do not grow into nearby tissues or spread to distant parts of the body. If they need to be treated, the patient can usually be cured with surgery.
Hemangioma
The most common type of benign liver tumor, hemangiomas, starts in blood vessels. Most hemangiomas of the liver cause no symptoms and do not need treatment. But some may bleed and need to be removed with surgery.
Hepatic edema
Hepatic adenoma is a benign tumor that starts from hepatocytes (the main type of liver cell). Most cause no symptoms and do not need treatment. But some eventually cause symptoms, such as pain or a lump in the abdomen (stomach area) or blood loss. Because there is a risk that the tumor could rupture (leading to severe blood loss) and a small risk that it could eventually develop into liver cancer, most experts will usually advise surgery to remove the tumor if possible.
Using certain drugs may increase the risk of getting these tumors. Women have a higher chance of having one of these tumors if they take birth control pills, although such an event is rare. Men who use anabolic steroids may also develop these tumors. Adenomas may shrink when these drugs are stopped.
Focal nodular hyperplasia
Focal nodular hyperplasia (FNH) is a tumor-like growth made up of several cell types (hepatocytes, bile duct cells, and connective tissue cells). Although FNH tumors are benign, they might cause symptoms. It can be difficult to tell them apart from true liver cancers, and doctors sometimes remove them when the diagnosis is unclear.
Both hepatic adenomas and FNH tumors are more common in women than in men.
Overview
Causes
- Long-term hepatitis B and hepatitis C infection are linked to liver cancer because they often lead to cirrhosis. Hepatitis B can lead to liver cancer without cirrhosis.
- Excessive alcohol use.
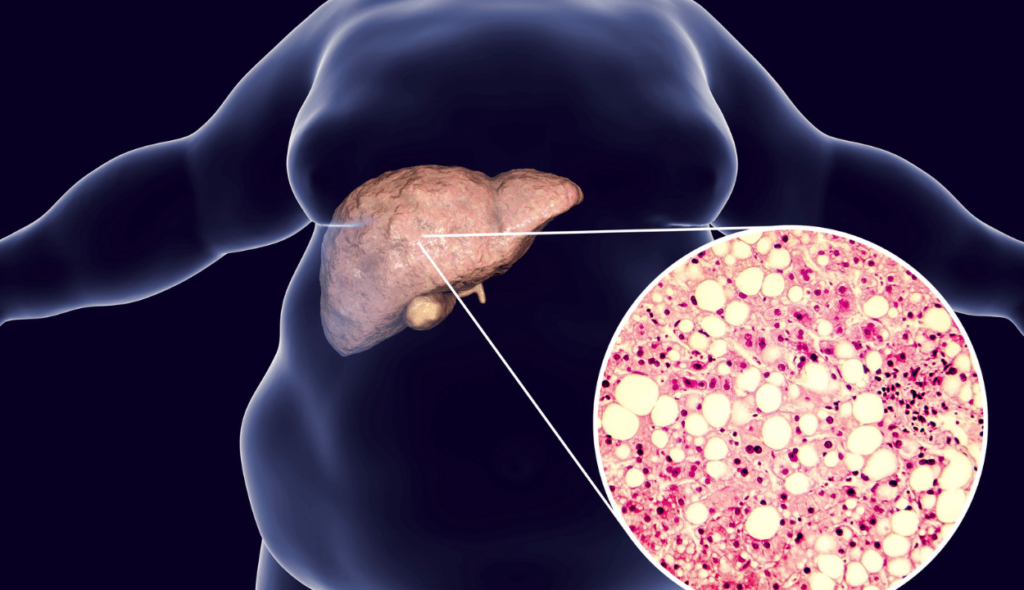
- Obesity and diabetes are closely associated with a type of liver abnormality called nonalcoholic fatty liver disease (NAFLD) that may increase the risk of liver cancer, especially in those who drink heavily or have viral hepatitis.
- Certain inherited metabolic diseases.
- Environmental exposure to aflatoxins.
- Many other liver diseases, including autoimmune diseases like PBC and other rare diseases such as tyrosinemia, alpha-1-antitrypsin deficiency, porphyria cutanea tarda, glycogen storage disease, and Wilson disease, can lead to cirrhosis, which increases the risk of liver cancer.
Doctors aren’t sure why some people get liver cancer while others don’t. However, there are certain factors that are known to increase the risk of developing liver cancer:
- Liver cancer is more common in people over age 50.
- A long-term hepatitis B or C infection can severely damage your liver. Hepatitis is spread from person to person through direct contact with the bodily fluids of an infected person, such as their blood or semen. It may also be passed from mother to child during childbirth. You can lower your risk for hepatitis B and C by using protection during sexual intercourse. There’s also a vaccine that can protect you against hepatitis B.
- Having two or more alcoholic beverages every day over many years increases your risk for liver cancer.
- Cirrhosis is a form of liver damage in which healthy tissue is replaced by scarred tissue. A scarred liver can’t function properly and may ultimately lead to numerous complications, including liver cancer. Long-term alcohol abuse and hepatitis C are the most common causes of cirrhosis in the United States. The majority of Americans with liver cancer have cirrhosis before they develop liver cancer.
- Exposure to aflatoxin is a risk factor. Aflatoxin is a toxic substance produced by a type of mold that can grow on peanuts, grains, and corn. In the United States, food-handling laws limit widespread exposure to aflatoxin. Outside of the country, however, aflatoxin exposure can be high.
- Diabetes and obesity are also risk factors. People with diabetes tend to be overweight or obese, which can cause liver problems and increase the risk for liver cancer.
Steps to reduce the risk of liver cancer include:
- Regularly see a doctor who specializes in liver disease
- Talk to your doctor about viral hepatitis prevention, including hepatitis A and hepatitis B vaccinations
- Take steps to prevent exposure to hepatitis B and hepatitis C. You can find out more about how to prevent hepatitis B here and how to prevent hepatitis C here.
- If you have cirrhosis or chronic liver disease, follow your doctor’s recommendations for treatment and be screened regularly for liver cancer
- If you are overweight or obese, diabetic, or drink heavily, talk to your doctor
Symptoms
Diagnosis
The diagnosis of liver cancer begins with a medical history and a physical examination. Make sure to tell your doctor if you have a history of long-term alcohol abuse or a chronic hepatitis B or C infection.
Diagnostic tests and procedures for liver cancer include the following:
- Liver function tests help your doctor determine the health of your liver by measuring levels of proteins, liver enzymes, and bilirubin in your blood.
- The presence of alpha-fetoprotein (AFP) in the blood can be a sign of liver cancer. This protein is usually only produced in the liver and yolk sac of babies before they’re born. AFP production normally stops after birth.
- Abdominal CT or MRI scans produce detailed images of the liver and other organs in the abdomen. They can allow your doctor to pinpoint where a tumor is developing, determine its size, and assess whether it has spread to other organs.
Liver Biopsy
Another diagnostic test available is a liver biopsy. A liver biopsy involves removing a small piece of liver tissue. It’s always done using anesthesia to prevent you from feeling any pain during the procedure.
In most cases, a needle biopsy is performed. During this procedure, your doctor will insert a thin needle through your abdomen and into your liver to obtain a tissue sample. The sample is then examined under a microscope for signs of cancer.
A liver biopsy might also be performed using a laparoscope, which is a thin, flexible tube with an attached camera. The camera allows your doctor to see what the liver looks like and to perform a more precise biopsy. The laparoscope is inserted through a small incision in the abdomen. If tissue samples from other organs are needed, your doctor will make a larger incision. The procedure is called a laparotomy.
If liver cancer is found, your doctor will determine the stage of the cancer. Staging describes the severity or extent of the cancer. It can help your doctor determine your treatment options and your outlook. Stage 4 is the most advanced stage of liver cancer.
Treatment and Management
How is liver cancer treated ?
Treatment for liver cancer varies. It depends on:
- the number, size, and location of the tumors in the liver
- how well the liver is functioning
- whether cirrhosis is present
- whether the tumor has spread to other organs
Your specific treatment plan will be based on these factors. Liver cancer treatments may include the following:
Proton therapy
Proton therapy has proved to be an excellent choice of treatment for non-metastatic liver cancer. In many of the cases, it is seen that the tumor goes away completely after proton therapy.
Hepatectomy
A hepatectomy is performed to remove either a portion of the liver or all of the liver. This surgery is usually done when the cancer is confined to the liver. Over time, the remaining healthy tissue will regrow and replace the missing part.
Liver Transplant
A liver transplant involves replacing the entire diseased liver with a healthy liver from a suitable donor. A transplant can only be done if the cancer hasn’t spread to other organs. Medicines to prevent rejection are given after the transplant.
Ablation
Ablation involves the use of heat or ethanol injections to destroy the cancer cells. It’s performed using local anesthesia. The anesthesia numbs the area to prevent you from feeling any pain. Ablation can help people who aren’t candidates for surgery or a transplant.
Chemotherapy
Chemotherapy is an aggressive form of drug therapy that destroys cancer cells. The medications are injected intravenously, or through a vein. In most cases, chemotherapy can be given as an outpatient treatment. Chemotherapy can be effective in treating liver cancer, but many people experience side effects during treatment, including vomiting, decreased appetite, and chills. Chemotherapy can also increase your risk of infection.
Radiation Therapy
Radiation therapy involves the use of high-energy radiation beams to kill cancer cells. It can be delivered by external beam radiation or by internal radiation. In external beam radiation, the radiation is aimed at the abdomen and chest. Internal radiation involves the use of a catheter to inject tiny radioactive spheres into the hepatic artery. The radiation then destroys the hepatic artery, a blood vessel that supplies blood to the liver. This procedure decreases the amount of blood flowing to the tumor. When the hepatic artery is closed off, the portal vein continues to nourish the liver.
Targeted Therapy
Targeted therapy involves the use of medications that are designed to hit cancer cells where they’re vulnerable. They decrease tumor growth and help shut down blood supply to the tumor. Sorafenib (Nexavar) has been approved as targeted therapy for people with liver cancer. Targeted therapy can be helpful for people who aren’t candidates for a hepatectomy or liver transplant. However, targeted therapy can have significant side effects.
Embolization and Chemoembolization
Embolization and chemoembolization are surgical procedures. They’re done to block off the hepatic artery. Your doctor will use small sponges or other particles to do this. The procedure reduces the amount of blood flowing to the tumor. In chemoembolization, your doctor injects chemotherapy drugs into the hepatic artery before the particles are injected. The blockage created keeps the chemotherapy medications in the liver for a longer period.
CAR T-Cell therapy for treatment of liver cancer
A recently created immunotherapy for the treatment of tumors is called chimeric antigen receptor-engineered T-cell (CAR-T) therapy. Its usage has been investigated in the treatment of solid tumors, such as liver cancer, because CAR-T therapy has demonstrated remarkable efficacy in treating CD19-positive hematological malignancies.
The application of CAR T-Cell therapy has started, and this has given new hope to patients suffering from late-stage liver cancer.