CAR T-cell treatment from IASO Biotherapeutics receives new FDA approval
Feb 2023: IASO Biotherapeutics’ investigational CAR T-cell therapy for relapsed or refractory multiple myeloma (RRMM), CT103A, has received fast track and regenerative medicine advanced therapy designations from the U.S. Food and Drug Administration (FDA), according to the firm.
These designations add to the treatment’s previous year’s orphan drug designation from the regulatory body.
These designations, which offer financial and regulatory support, are meant to hasten the development of drugs that have the potential to treat serious, life-threatening, or uncommon diseases for which there are currently insufficient treatments.
“Leveraging its … innovative product pipeline [and] integrated manufactural and clinical capabilities, IASO aims to deliver transformative, curable and affordable therapies that fulfill unmet medical needs to the patients in China as well as around the world,” the company said in its announcement.
US trial of CT103A expected in May
Fast track status lets you go through a rolling review and see if you qualify for faster approval and a priority review. Rolling review means that a company can send in parts of a regulatory application as they are ready, instead of waiting until all of the parts are done before the agency can look at the application.
Accelerated approval, also called “conditional approval,” is given to treatments whose immediate availability fills a medical need that hasn’t been met yet, as long as early evidence shows that the benefits of the treatment outweigh the risks.
With an RMAT designation, you can talk to the FDA early, often, and up close. In the case of an accelerated approval, the clinical evidence needed to confirm the therapy’s benefits and get a full approval may come from sources other than the traditional confirmatory clinical trial, which usually saves time and money.
So far, CT103A has only been tried out on myeloma patients in China, where it was deemed a breakthrough therapy and is now being reviewed quickly. There, IASO and Innovent Biologics are working together to make CT103A.
In December, the FDA approved IASO’s application for an investigational new drug. This meant that CT103A could be used in clinical trials in the U.S.
A Phase 1b clinical trial (NCT05698303) will test the treatment on up to 12 adults with RRMM to see how safe and effective it is. The study will be done at the MD Anderson Cancer Center at the University of Texas in Houston, Texas. It is expected to begin in May.
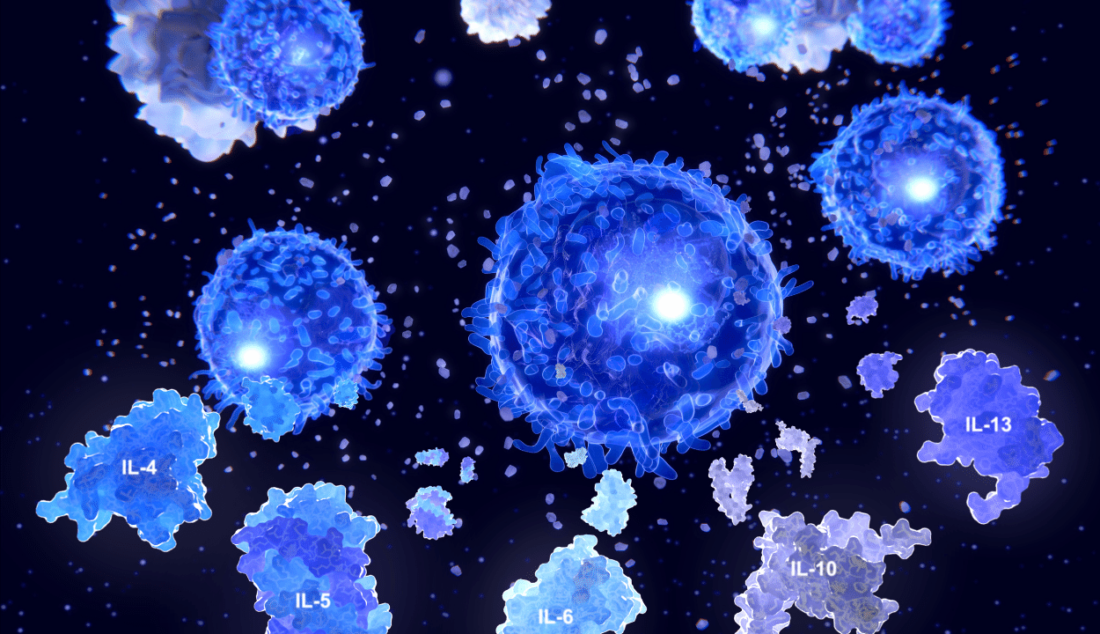
Chimeric antigen receptor (CAR) T-cell therapy works by making it easier for T-cells, which are a type of immune cell that can fight cancer, to find and attack cancer cells.
Collecting a patient’s T-cells and changing them in the lab to make a receptor, or CAR, that recognises specific proteins on cancer cells is the main idea behind this method. When these engineered cells are put back into the body, they should find and kill cancer cells without hurting the body’s healthy cells.
CT103A goes after a protein called B-cell mature antigen that is only found in cancer cells (BCMA). It also has a small piece of a human antibody that is meant to lower the chance that the body’s immune system will attack the therapy. This is a common problem with CAR T-cell therapies that can make it hard to re-dose them if a person’s cancer comes back.
In an early pilot Phase 1 trial (ChiCTR1800018137) in China, 18 people with RRMM were given the treatment. After about a year, all of them had a response to the treatment. Almost three-quarters (72,2%) had a complete response or better, which means that their tumour was gone.
Till date, IOSA’s CAR T-cell therapy only tested in China
After that, a Phase 1/2 trial called FUMANBA-1 (NCT05066646) was started in China to test the safety and effectiveness of CT103A in up to 132 adults with RRMM.
Last year, at the European Hematology Association Research Conference, a presentation was given called “Updated Phase 1/2 Data of the Safety and Efficacy of CT103A, Fully-Human BCMA-Directed CAR-T Cells in Relapsed/Refractory Multiple Myeloma.” This was based on data from the first two phases of the study.
As of January 21, 2022, CT103A had been used to treat 79 people, and the average time for follow-up was nearly 10 months.
These patients had already been through a median of five lines of treatment, some of which were immunomodulatory drugs, proteasome inhibitors, and CD38 inhibitors. Twelve (15.2%) of them had already been treated with non-human BCMA-targeted CAR-T cell therapy.
After a median of 16 days of treatment, the results showed that most patients (94.9%) had at least a partial response. This included 68.4% of patients who had a complete response or better and 89.9% of patients who had a very good partial response or better.
Ten people with extramedullary myeloma, a type of cancer that grows outside of the bone marrow, all got better from the treatment. All of these people got better after treatment, and 90% of them got better or completely better.
The response rate for the 12 people who had CAR T-cell therapy before was 75%, and 41.7% of those people had a complete response or better.
Out of the whole group of 79 patients, 92.4% were also negative for minimal residual disease, or the small number of cancer cells that can sometimes remain after treatment and cause the disease to come back.
The safety profile of CT103A was good and easy to handle.
Most patients (94.9%) had cytokine release syndrome, which is an immune response that can be dangerous and is often seen with CAR T-cell therapies. But most of the time, these reactions were mild or moderate and lasted about five days.
Immune effector cell-associated neurotoxicity syndrome, a serious immune response that affects the nervous system, was seen in two people. Their symptoms were mild or moderate and went away.
In general, CT103A did not cause immune responses that were against the treatment, though 16.5% of patients tested positive for antibodies against CT103A.
In a Phase 1 FUMANBA-2 trial (NCT05181501), up to 20 newly diagnosed, high-risk multiple myeloma patients are being tested to see if CT103A could help them.
Susan Hau is a distinguished researcher in the field of cancer cell therapy, with a particular focus on T cell-based approaches and cancer vaccines. Her work spans several innovative treatment modalities, including CAR T-cell therapy, TIL (Tumor-Infiltrating Lymphocyte) therapy, and NK (Natural Killer) cell therapy.
Hau's expertise lies in cancer cell biology, where she has made significant contributions to understanding the complex interactions between immune cells and tumors.
Her research aims to enhance the efficacy of immunotherapies by manipulating the tumor microenvironment and exploring novel ways to activate and direct immune responses against cancer cells.
Throughout her career, Hau has collaborated with leading professors and researchers in the field of cancer treatment, both in the United States and China.
These international experiences have broadened her perspective and contributed to her innovative approach to cancer therapy development.
Hau's work is particularly focused on addressing the challenges of treating advanced and metastatic cancers. She has been involved in clinical trials evaluating the safety and efficacy of various immunotherapy approaches, including the promising Gamma Delta T cell therapy.
- Comments Closed
- February 21st, 2023





China, IASO Biotherapeutics, multiple myeloma
CancerFax is the most trusted online platform dedicated to connecting individuals facing advanced-stage cancer with groundbreaking cell therapies.
Send your medical reports and get a free analysis.
🌟 Join us in the fight against cancer! 🌟
Привет,
CancerFax — это самая надежная онлайн-платформа, призванная предоставить людям, столкнувшимся с раком на поздних стадиях, доступ к революционным клеточным методам лечения.
Отправьте свои медицинские заключения и получите бесплатный анализ.
🌟 Присоединяйтесь к нам в борьбе с раком! 🌟