
CAR T-Cell Therapy for neuroendocrine tumors
Neuroendocrine tumors (NETs) are rare malignancies that arise from neuroendocrine cells, which are responsible for producing hormones.
These tumors can occur in various parts of the body, including the lungs, pancreas, and gastrointestinal tract. While some NETs are slow-growing, others can be aggressive and metastatic.
However, advancements in immunotherapy, specifically CAR T-cell therapy, have opened new avenues for treatment.
What Are Neuroendocrine Tumors and Their Types?
Neuroendocrine tumors (NETs) represent a heterologous group of cancers arising from neuroendocrine cells, whose features combine aspects of both hormone-secreting and nerve cells. They produce hormones leading to specific symptoms commonly known as carcinoid syndrome. NETs have the ability to arise in nearly any organ, but the majority are discovered within the gastrointestinal tract, pancreas, and lung.
Types of Neuroendocrine Tumors:
Gastroenteropancreatic Neuroendocrine Tumors (GEP-NETs): These are the most common type of NETs, primarily found in the digestive tract and pancreas.
Pulmonary NETs: Found in the lungs, these tumors are further divided into typical carcinoids and atypical carcinoids, with the latter being more aggressive.
Pheochromocytomas and Paragangliomas: Tumors arising from the adrenal glands or along nerve tissue, often leading to excessive hormone production.
Medullary Thyroid Carcinoma (MTC): A form of thyroid cancer originating from parafollicular C cells.
Merkel Cell Carcinoma: A rare and aggressive form of skin cancer that develops from neuroendocrine cells in the skin.
Each type of NET presents unique challenges in diagnosis and treatment, emphasizing the need for targeted therapies like CAR T-cell therapy.
CAR T Cell therapy
It is one of the groundbreaking forms of immunotherapy that puts to bear the power of a person’s own immune system against cancer. This treatment involves making T cells carry a synthetic receptor known as CAR that specifically makes them recognize tumor-specific antigens expressed by cancer cells, and on infusing them back into the body, these engineered T cells can recognize and destroy cancer cells with remarkable precision.
The process includes:
T Cell Extraction: Collecting T cells from the patient through apheresis.
Genetic Modification: Engineering the T cells to express a CAR, which is designed to target specific antigens on tumor cells.
Expansion: Multiplying the CAR T cells in a laboratory.
Infusion: Administering the modified T cells back into the patient.
Once inside the body, CAR T cells seek out and eliminate cancer cells expressing the targeted antigen.
CAR T-cell therapy has greatly succeeded in hematologic malignancies, including leukemia and lymphoma. The same cannot be said for its use in solid malignancies such as breast and lung cancer. Such is mainly attributed to the heterogeneity of tumors, the immunosuppressive nature of the tumor microenvironment, and the lack of targetable antigens. Many researchers are pursuing CAR T-cell therapy in the treatment of breast cancer with attention to HER2, MUC1, and FRα for specificity and potency.
Though promising, CAR T-cell therapy comes with potential side effects, including cytokine release syndrome (CRS) and neurotoxicity. Studies are underway to improve safety and efficacy, including the development of bispecific CARs and armored CAR T cells. As the clinical trials advance, CAR T-cell therapy promises to revolutionize cancer treatment and provide hope to patients with aggressive or treatment-resistant cancers.
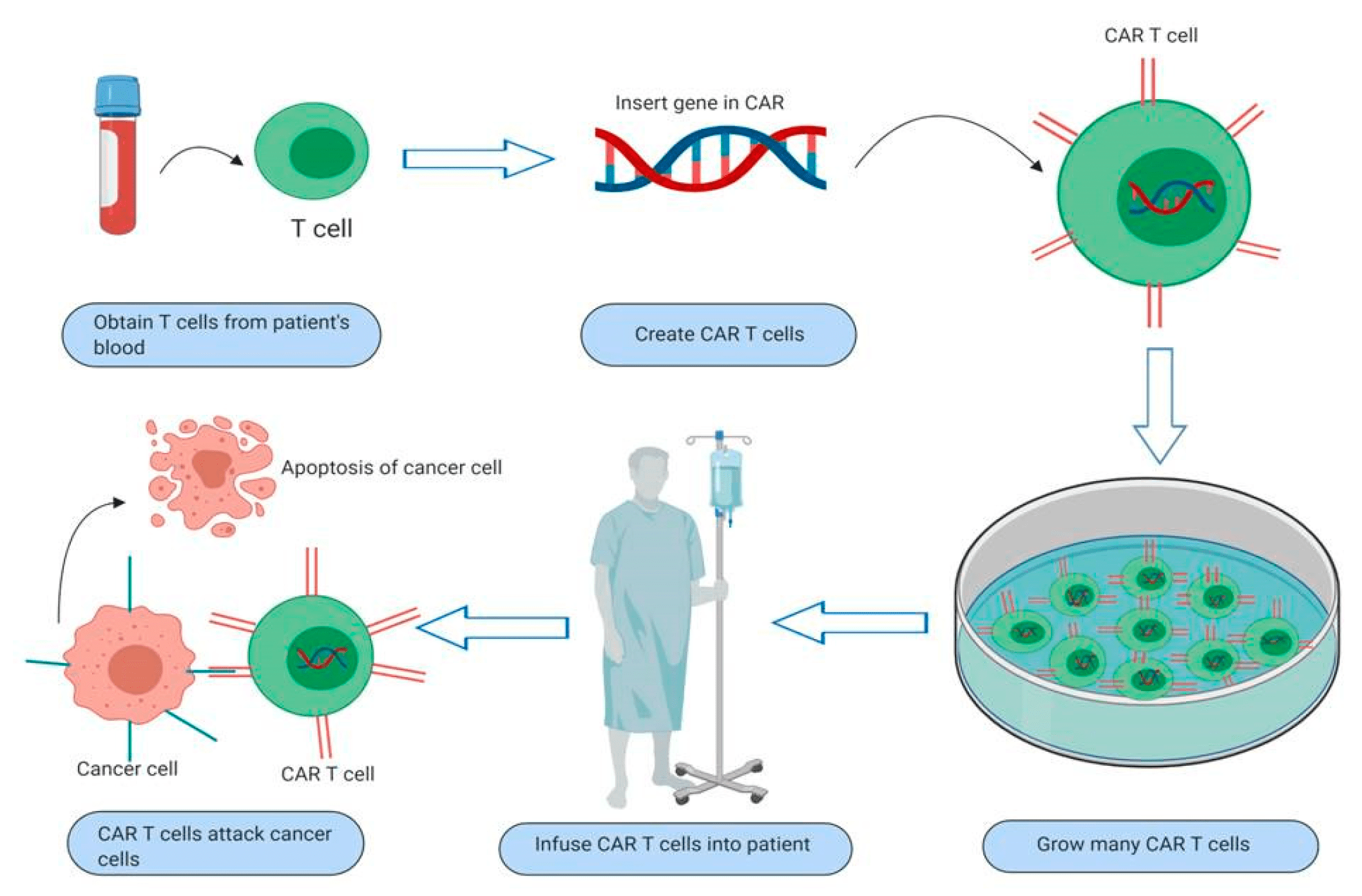
Pic: Working of CAR T Cell therapy
Challenges in NETs Treatment
Unlike hematologic cancers, solid tumors such as NETs pose unique challenges for CAR T-cell therapy. Key issues include:
Heterogeneity: NETs exhibit diverse genetic and molecular profiles.
Lack of Universal Targets: Identifying specific antigens for NETs remains difficult.
Tumor Microenvironment: NETs create an immunosuppressive environment that hinders T-cell activity.
Toxicity Management: CAR T-cell therapy may cause cytokine release syndrome (CRS) or neurotoxicity, requiring careful management.
Target Antigens for CAR T-Cell Therapy in NETs
Several antigens have been explored for CAR T-cell therapy in NETs, including:
Cytokeratin 19 (CK19)
Somatostatin Receptors (SSTRs)
CEA (Carcinoembryonic Antigen)
EpCAM (Epithelial Cell Adhesion Molecule)
Research efforts are underway to identify new, more specific antigens for targeted therapies.
Clinical Trials and Research Progress
Numerous clinical trials are investigating the safety and efficacy of CAR T-cell therapy for NETs. Early-phase studies have shown promising results in tumor regression and improved survival rates. Researchers are also exploring combination therapies, such as CAR T cells with immune checkpoint inhibitors, to enhance anti-tumor responses.
Advancements in China
China has become a front-runner in CAR T-cell research, with many institutions performing innovative trials for solid tumors such as NETs. Chinese scientists are taking advantage of cutting-edge genetic engineering methods and creating dual-targeting CAR T cells to deal with tumor heterogeneity. Innovations in the process of manufacturing have also decreased costs and increased patient access.
A number of Chinese hospitals and biotech firms have reported positive results in initial-stage trials of NETs with considerable tumor regression and tolerable side effects. All these advancements are helping shape CAR T-cell therapy globally.
Future Prospects
The future of CAR T-cell therapy for NETs looks promising with ongoing research focusing on:
Next-Generation CAR T Cells: Engineering T cells with enhanced persistence and reduced toxicity.
Personalized Therapy: Tailoring CAR T cells to individual tumor profiles.
Combination Therapies: Using CAR T cells alongside other immunotherapies and targeted drugs.
Improved Targeting: Identifying novel antigens and employing dual-targeting CAR T cells.
Conclusion
CAR T-cell therapy is a revolutionary treatment for neuroendocrine tumors. While there are still challenges, ongoing research, especially in nations such as China, is pushing the field forward. For patients with refractory or metastatic NETs, CAR T-cell therapy can provide a new glimmer of hope for better results.
Contact CancerFax for CAR T Cell Therapy
If you or your loved one is seeking CAR T-cell therapy for colorectal cancer or other solid tumors, contact CancerFax today. Our experts provide access to cutting-edge treatments, personalized guidance, and global medical partnerships. Visit CancerFax.com to learn more and explore your options for advanced cancer care.