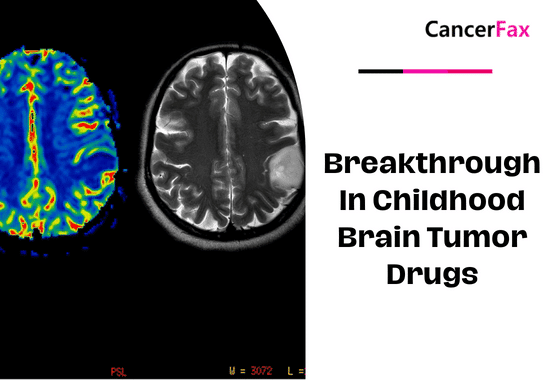
There is a big breakthrough in childhood brain tumor drug development. Children’s brain tumors are a more common malignant disease in children. Recent research has found that a new cocktail drug can treat common childhood brain tumors.
Cancer Cell” magazine recently announced that in the UK, about 400 children develop brain tumors each year, of which the prevalence of boys is slightly higher than that of girls.
Are we able to take advantage of the results of tumor gene testing and tailor-made treatments, a strategy often referred to as personalized medicine? This treatment strategy can produce very good results for patients with brain tumors.
Neural myeloblastoma (medulloblastoma) is one of the most common malignant tumors of the cerebellum. This brain tumor grows rapidly and most often occurs in children around the age of 5. Treatment options include surgery, radiation, and chemotherapy. Although great progress has been made in treatment methods and techniques, the success rate of treating myeloblastoma still lags far behind other children’s malignancies. In particular, myeloblastoma is a highly aggressive malignancy. Only 40% of patients with medulloblastoma survive, compared with other tumors of a less severe type-with a survival rate of more than 80%.
Researchers in the United States have discovered a new combination therapy for the treatment of highly aggressive neuroblastoma. In laboratory tests, the drug killed cancer cells without any toxicity to normal cells, and researchers hope to conduct clinical trials of the drug. Robert Wechsler-Reya, an adjunct professor at the Sanford Burnham Prebys Medical Institute, said: “Our goal is to confirm that the drug has low toxicity properties. Because doctors and patients in this case urgently require new clinical treatment options, we will soon apply the drug from the laboratory to clinical treatment.
By combining with other drugs, new compounds that inhibit tumors are screened in vitro and in vivo.
Clinical trials for neuroblastoma are often very challenging because of the limited number of patients. In addition, coupled with the variability of the disease, most treatments are only effective for one subtype of patient. Understanding which patients will respond to this treatment is one of the main goals of the trial.
“If we can develop tailor-made treatments based on tumor genes-a strategy commonly referred to as individualized treatment-this could bring a huge gospel to patients with certain tumors.”
There are four distinct types of neuroblastoma, and patients with a third group of tumors have the worst prognosis—only 40% of patients survive long-term. In contrast, the long-term survival of other neuroblastomas is relatively optimistic, and about 80% of patients can survive long-term.
Most of the third group of patients with neuroblastoma have high expression of the MYC oncogene, which is the cause of uncontrollable cell division and the formation of tumors.
There was a study on mice with a third type of neural tube cell tumors that showed histone deacetylase inhibitors (HDACIs) and phosphatidylinositol 3-kinase inhibitors (PI3KIs) might stop mice and people from making neurotubular glioblastomas without doing too much damage to normal cells.
We found several histone deacetylase inhibitors that can kill MYC oncogene-activated neural tube cell tumors without harming normal cell agents (HDACIs),” said Pei Yanxin, an assistant professor at the National Children’s Medical Center in Washington, D.C.
The most effective of these compounds is panobinostat, which has entered clinical trials in other types of cancer, but has not yet been tested on neuroblastoma.” Dr. Kun-Wei, a postdoctoral researcher at Stanford University, added: “Several other studies have revealed that the mechanism of action of panobinostat is to promote the activation of the FOXO1 gene that can interfere with the oncogenes of MYC.
Phosphatidylinositol 3-kinase inhibitors (PI3KIs) are also thought to have the effect of activating the FOXO1 gene. We hypothesized that panobinostat and phosphatidylinositol 3-kinase inhibitors (PI3KIs) could work together to block cancer cell survival.
“It is true that the combined treatment of these two drugs can significantly increase the survival of patients with tumors carrying the MYC gene compared to using a single drug alone.”